Pacemaker implantation is one of the few high impact interventions done by cardiologists.Traditionally , RV apex was paced for many decades with tined or screwing leads. Serious concern was raised in recent years about the ideal site of pacemaker lead position. .Today, some argue pacing RV from RV apex is a electro-physiological crime (Of-course it appears more of hyped up fear ! )
What is the concern with RV apical pacing ?
RV apical pacing is unphysiological .To mimic physiology we have to move the lead as cranial as possible within RV. (*Obviously pacing anywhere in RV is non-physiological .Best would be atrial pacing . This is possible only in sinus node dysfunction with Intact AV conduction.) Hence RVOT and mid septal pacing was proposed and practiced as a relatively more physiological site as the spike could capture the natural conduction system early and ventricle is activated from above down.
How to localise the RV lead in mid septum ?
Inter ventricular septum , hardly occupies an area of 5/5 sq cm with a complex structure , shape and alignment with RV and LV cavity .In pathological states it can further get distorted. To catch it’s profile in fluoroscopy and imagine the plane requires a mind of “cardiac architect”.So, to locate the IVS various views are suggested. Currently LAO 40 is typically used for fixing mid septal position. In midseptal position ECG is expected to show small q in lead 1 and AVL. QRS axis will be more left .We seemed to agree with this.
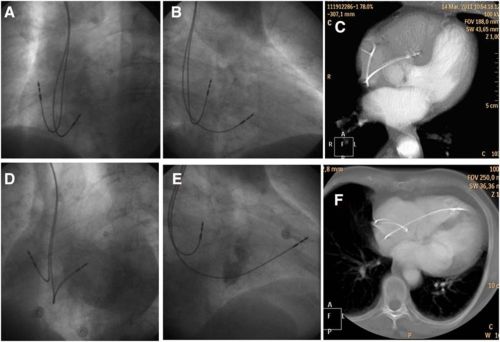
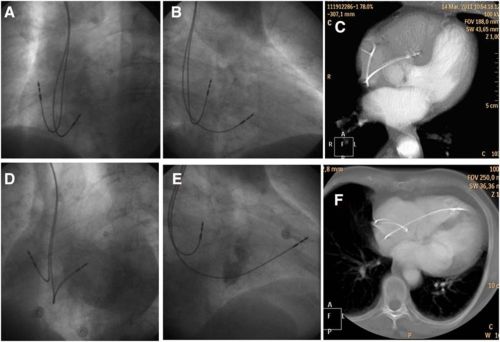
- Image courtesy: Pavel Osmancik Circulation: Arrhythmia and Electrophysiology. 2013; 6: 719-725 Fluoroscopic examples of 2 patients. One with correct lead placement in the septum (A–C) and the other with the lead placed in the anterior wall (D–F). See the similarity of the left anterior oblique 40 view, the difference of the right anterior oblique 30 and the location of the lead on computed tomography image.
And suddenly this paper from the picturesque city of Prague , Czechoslovakia throws a stunner.
What we have been thinking as mid septal pacing with LAO protocol turns out to be anterior RV pacing in 60% of times.The study showed LA0 40 view failed to differentiate anterior RV pacing from mid septal pacing .CT scan correlates have documented this . Further ,we have never given a thought to the wayward trabecuale coming across mid septal zone. It has happened time and again (Atleast i have witnessed) the lead would just fall short of IVS and get screwed in the trabeculae with high risk for dislodgement . RAO 30 view consistently separates the mid septal lead from anterior RV position.It is suggested a carefully done per-procedure echo would also be useful in locating the lead tip .
What hemodynamic implication of mid vs RV anterior pacing ?
Could be significant . No reliable data available. It s tempting to think the hemodynamic inadequacies of an improperly placed mid septal RV pacing may not be different from a conventional RV apex pacing .
Final message
The complex shape of RV and IVS in fluoroscopy can fool us. If you really want to pace the mid septum, please ensure with multiple views and confirm with RAO 30 . Also remember echocardiography is not a forbidden tool for localising pacemaker lead.
Reference
1.The Insufficiency of Left Anterior Oblique and the Usefulness of Right Anterior Oblique Projection for Correct Localization of a Computed Tomography–Verified Right Ventricular Lead Into the Midseptum Pavel Osmancik, Petr Stros, Dalibor Heart 2013; 6: 719-725
Read Full Post »