It would be silly to remind, it’s the same five liters of blood, that circulates across, both the arterial and venous system. But, its journey one away from the heart, and the other towards the heart are strikingly different. They are subjected to various hemodynamic forces, travels different terrains, at different speeds, thousands of kilometers of microvasculature along the cardiovascular highway, yet merging with each other every 15 seconds or so, at the pulmonary junction box. Have a look at the following images, to understand the distribution of the blood volume.
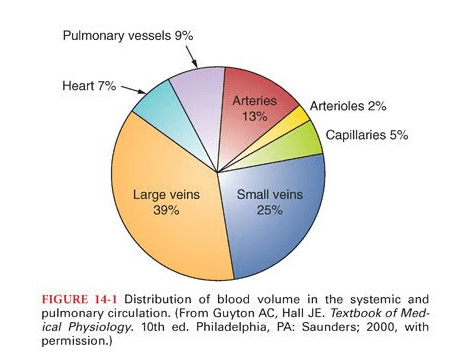

The first image is taken from the maverick physiologist Dr. Guyton’s textbook of physiology, and the second one from the equally famous Dr. Ganong’s. Both images depict the distribution of blood volume, the corresponding pressures, and velocity. Every cardiology fellow should recall these two images even in their sleep. Also mind, they circulate around the body, lifelong without clotting or bleeding, assisted by the right balance of pro and antithrombotic forces.
Why some of patient’s blood is more likely to get frozen ?
Logic would suggest venous thrombosis should be more prevalent than arterial thrombosis at any point of time and location. This is due to the slowness of the circulation and the enormous volume within the venous reservoir. But is this the clinical reality? It is indeed true, that incidence of minor venous thrombosis exceeds arterial thrombosis. Since venous thrombosis often gets lysed or get stuck in the lungs, it’s frequently under-recognized. Arterial thrombosis causes more damage in an important sense, as it leads to target organ ischemia.
Apart from hemodynamic factors, the 200 year old Virchow’s triad is very much alive. The vessel wall integrity, intrinsic defects in the coagulation and anticoagulant/fibrinolytic molecules, the genetic susceptibility are the important determining factors. The RBC and platelet behaviour too changes, in high and low pressure environments.
How to diagnose a patient who is in a procoagulant state?
The topic is so complex .Many things are still poorly understood. We should have a checklist of all systemic conditions that can cause increased risk of thrombus. We know pregnancy is inherently a procoagulant state, as is manifest or concealed malignancy.
What we normally do ?
It is very easy to tick the coagulation profile/panel slip and pass it on to the nursing staff. Some of us take another easy route, referring such patients to a rheumatologist for the risk-stratifying job. This is probably because we strongly believe SLE and connective tissue disorders are the first culprits.
I think we need to engage the hematologist more often because thrombosis is not only due to excess coagulation. It is also due to a lack of enough circulating anticoagulants. (As a cardiologist, sometimes I feel awkward. to call myself an expert of the circulatory system, with almost zero knowledge of how the blood clots or dissolves.) This article tries to differentiate the risk factors operative on the venous and arterial sides. It is only a gross attempt; many risk factors are invisible and are common between arterial and venous thrombus.
For a detailed analysis of Sydney criteria /ACR-EULAR (Reference 7 )
How to treat pro-coagulant state?
Fortunately, identifying the thrombosis prone patients is complex , but the treatment is fairly simple. We have only few options: Aspirin, Warfarin, and NOACs *We need to choose one of them. The general rule is aspirin doesn’t work much on the venous side. I don’t know how far this is really true. (It has something to do with the shearing force of platelets? ) However, in obstetrics, the placental circulation is full of low pressure venous plexus where Aspirin is used as a norm.
Between Warfarin and NOACs, there is absolutely no doubt Warfarin is the clear winner on the arterial side. Because of monitoring issues and fear of bleeding, we are compelled to switch to NOACs in many situations. Beware, think twice before prescribing NOAC for prophylaxis against arterial thrombus. The venous side does not have much difference in choice. *Heparin (& its glamor sibling LMWH) is a unique molecule, which has ability to work on both arterial and venous sides.
References
Postamble
The article doesn’t discuss the intra vascular metals, wires, devices, valves, pacemakers , related thrombosis. Here there is a known trigger. It is possible, they also influenced by the baseline factors of pro-coagulation discussed above.


