1.Is systemic HT an advantage ?so that high pressure head aids in pushing the blood across the lesion. ?
I don’t know whether I can say Yes*, physiologically, the high proximal pressure and low distal pressure help maintain the flow. The distal drop happens due to the tightness of the lesion itself, but that is counterproductive, unless tone of the distal microvascular bed is intact and dilates fully.
*Mind you, IABP during cardiogenic shock, essentially does this – keep the coroanry diastolic pressure high.
However, there are significant caveats.
There is law of diminishing Returns : In a 90% lesion, the resistance is so high that even elevated Pa may not substantially increase flow due to the fixed obstruction. Hypertension increases left ventricular afterload, raising myocardial oxygen demand. In a 90% LAD lesion with compromised flow, this can worsen ischemia, outweighing any flow benefit from higher pressure.
2.What happens to trans-lesion flow during hypotension ?
This has direct implications when a patient with a significant lesion develops hypotension due to a systemic cause like dehydration or postoperative hypovolemia. We have often observed transient ST/T changes in a postoperative patient that may or may not lead to full-blown ACS.
To know what exactly happens across a lesion, we need to understand coronary autoregulation and its limits. Coronary autoregulation maintains stable myocardial blood flow despite changes in coronary perfusion pressure. Its limits and range are as follows. .
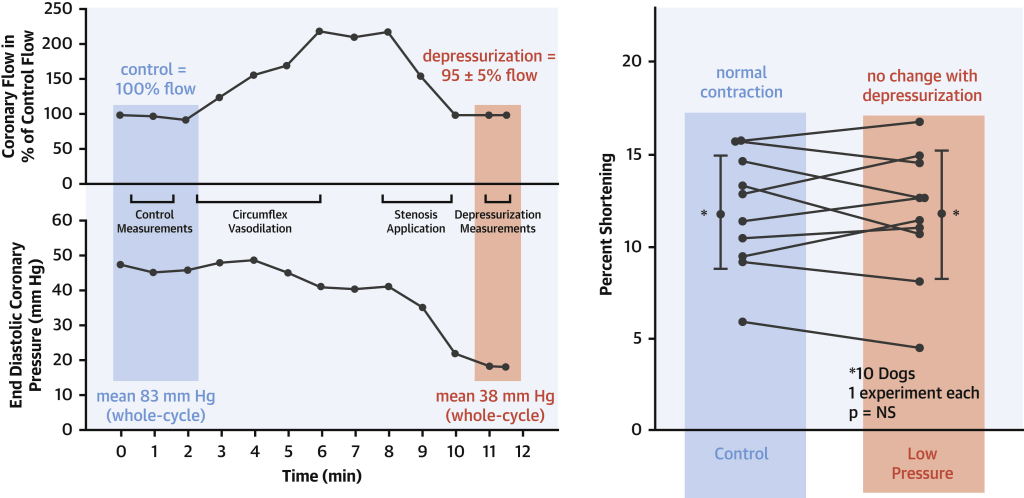
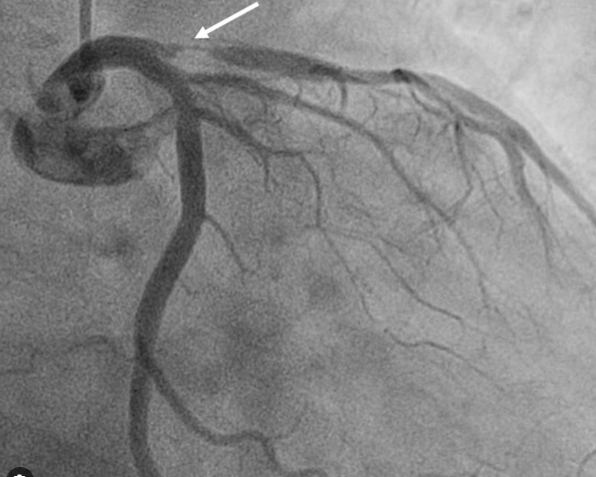
The famous dog experiment on the coronary flow on depressurisation (Ref 2)
Range of Autoregulation: In healthy coronary arteries, autoregulation operates effectively between perfusion pressures of approximately 50–60 mmHg to 120–140 mmHg. Within this range, vascular smooth muscle in coronary arterioles adjusts resistance to maintain near-constant blood flow.Lower Limit: Below 50–60 mmHg, autoregulation fails, and blood flow becomes pressure-dependent. This can lead to ischemia, especially in the subendocardium, which is most vulnerable due to higher oxygen demand.Upper Limit: Above 120–140 mmHg, maximal vasodilation is reached, and further increases in pressure do not significantly increase flow.
However , we don’t know how this autoregulatory biological servo control, is tampered in the presence of a single or a tandem lesions.
3.How does FFR gets altered during exertion in such lesion ?
We have very limited data available on this and are essentially ignorant . FFR during exertion typically decreases compared to rest due to the amplified pressure gradient across the stenosis driven by increased flow demand and limited reserve.However collaterals can mitigate this fall in FFR.
Final message
Putting a stent across 90% lesion surely is a childish task, when compared to understanding complex hemodynamic vortices that happen across it.
Reference