Transcatheter PDA (tcPDA) closure has become the preferred invasive option for hemodynamically significant PDA (hsPDA) in preterm infants after the recent FDA approval of dedicated devices . However we need to ensure that this powerful therapy is used selectively, based on true hemodynamic need, with proper expertise and infrastructure, and not as a routine response to any persistent duct. SCAI has come out with a new Position statement on this issue. (Ref 1)
Prematurity, PDA, and hemodynamic significance
Extremely premature infants have a high incidence of persistent PDA and are vulnerable chronic lung disease, pulmonary vascular disease, higher respiratory support, NEC, and mortality. Not all PDAs in this group warrant closure .Treatment is strictly reserved for hsPDA, where the left‑to‑right shunt clearly causes pulmonary overcirculation and/or systemic hypoperfusion. It is wise to note, medical therapy closes about two‑thirds of PDAs versus about one‑third without treatment, underscoring the importance of pharmacologic management alone.
Recognition of significant PDA : Clinical or Echocardiography ?
It is prudent, the selection for tcPDA should start with clinical assessment. It mainly goes with high ventilator or oxygen dependece attributed to shunt physiology, plus signs of systemic compromise despite optimal general care. Infants <28 weeks’ gestation, >10 days old, and still invasively ventilated in high‑risk units are potential candidates when these clinical features are present and expertise is available.
Limits of echocardiographic Indices
Echocardiographic parameters include, duct size, left‑heart volume loading, and holodiastolic flow reversal to define hsPDA . It must be emphasized Duct diameter alone correlates poorly with true hemodynamic impact. A large PFO or small ASD can decompress the left heart, blunting classic echo markers and masking a genuinely important shunt . Also , dynamic pulmonary vascular resistance, sepsis, systemic inflammation, renal dysfunction, may exaggerate the severity of an anatomically modest shunt, leading to unnecessary catheterization.
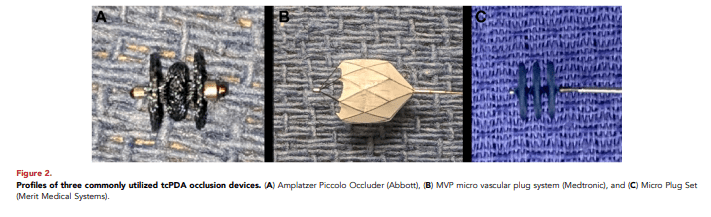
Some of the devices used in PDA closure. Piccolo, MVP and Micro-plug (Fraisse A, et al Front Pediatr. 2020 )
Priority of medical therapy before device closure
Pharmacologic closure with ibuprofen, indomethacin, or acetaminophen remains the recommended first‑line approach with a closure rate of 70% .
Final message
Transcatheter rather than surgical has become the definitive option when conservative or medical therapy fail. (Inspite of the fact, catheter access can be difficult in very small babies ) .However, the more important issue could be avoiding premature and unnecessary device closure in premature infants.
Reference : Link