“Half-baked knowledge is not better than fully-baked Ignorance“
LDL is portrayed as villain de-chief of Atheroscerlois and CAD. But, LDL with a 100 to 160 mg concentration, is in constant circulation, in a smooth manner serving other physiological vascular functions.
The forcible evidence that LDL can pierce an Intact endothelium is so huge no one can have the courage to dispute it. But, it doesn’t happen in the majority is the mysterious truth.
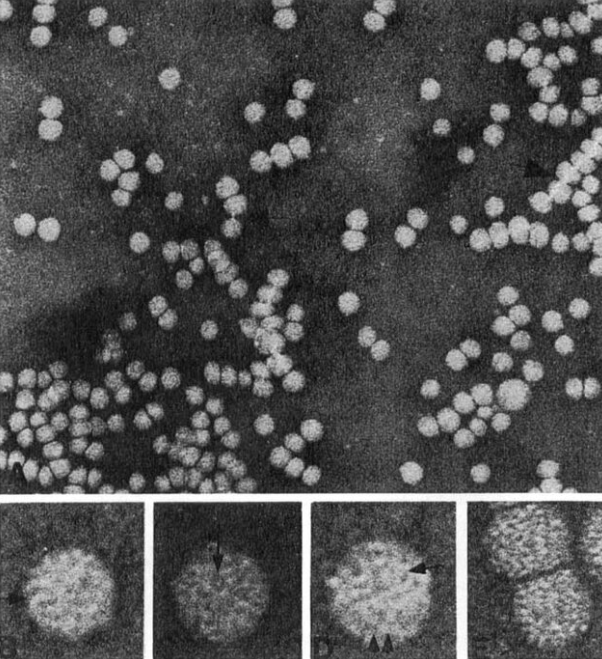
Electron microscopic picture of 20nm sized LDL molecules in circulation. They are not as frightening molecules as they are portrayed
What factors induce LDL to enter the endothelial gap junctions.?
Some facts
The diameter of LDL particles is about 20–30 nm which is much larger than that of gap-junctions (3–6 nm) between adjacent cells in continuous endothelium (Iuliano, Micheletta, & Violi, 2001). Hence, the only way for LDLs to cross the endothelium is through a process called caveolae-mediated transcytosis.
Contrary to the shout-out, LDL is not a true villain in all patients with CAD. It is something else, we aren’t aware of that keeps the LDL either passive or promotes its penetration.
There are at least five important factors.
1. Baseline Endothelial Integrity & vascular aging
2. Accelerated caveolae formation,
3,The shear stress of flowing BP .
4 .The associated diabetic basement membrane dysfunction.
5. Finally, the aggressiveness of native LDL molecule (Absolute levels of LDL are less important than we think . Please note, the much-researched South Asian metabolic syndrome has near normal LDL )
What we fail to acknowledge is the fact that our understanding of endothelial lipid interaction is based on poor-quality data . Meanwhile, the concept of endothelial-friendly LDL can’t be eliminated totally.
Final message
How many molecules of LDL enter endothelial breakpoints?
I am sure, no one can answer this question. In fact, this question need not be answered. Still, the PCSK blockers, the Inclisirons are the new armed weapons in anti LDL industry waiting hungrily to Invade the vasculature. What if these agents swallow good LDLs ?
Let us first clarify, the true invading potential of LDL before falling for these costly semi-annual subscription-based drugs. Meanwhile, HDL dysfunction with its Apo A2 interaction defects may be a more concerning issue than LDL-mediated injury is coming up.
Reference