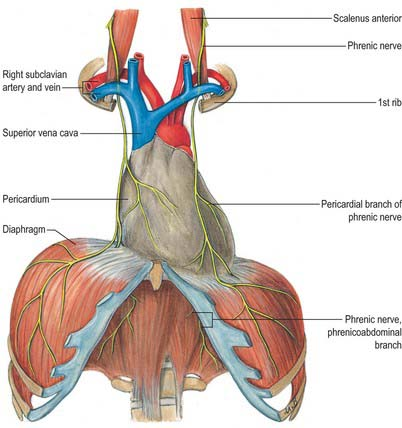
Phrenic nerve arises from C3, C4, C5 cervical spinal nerves ,but essentially from C4 . In the neck, it runs along the anterior scalene muscle, deep to the pre-vertebral fascia. It Enters the thoracic inlet posterior to the subclavian vein and anterior to the subclavian artery.
Does It traverse the Pericardial Space?
Contrary to my longstanding belief, realized just now, the phrenic nerve does not enter the pericardial cavity. Rather, It courses within the fibrous pericardium, between the fibrous pericardium (outer layer) and mediastinal pleura. Hence, it is extrapericardial but intimately related to the fibrous pericardium. (Yes, I was indeed a prof of cardiology, teaching students. Wish, I could learn cardiac anatomy from the scratch again)
Anyway, the fact that it runs outside the pericardium, doesn’t give any comfort to the electrophysiologists, both during epicardial and sub-endicardial ablations. It is worth noting the important differences in the course of right and left phrenic nerves.

Difference between right and left phrenic nerves anatomy

Understanding the anatomy of the phrenic nerve is crucial for both cardiac surgeons (of course they see with their eyes) and electrophysiologists. Phreni nerve injury or ablatio can lead to serious consequences.
Right phrenic nerve
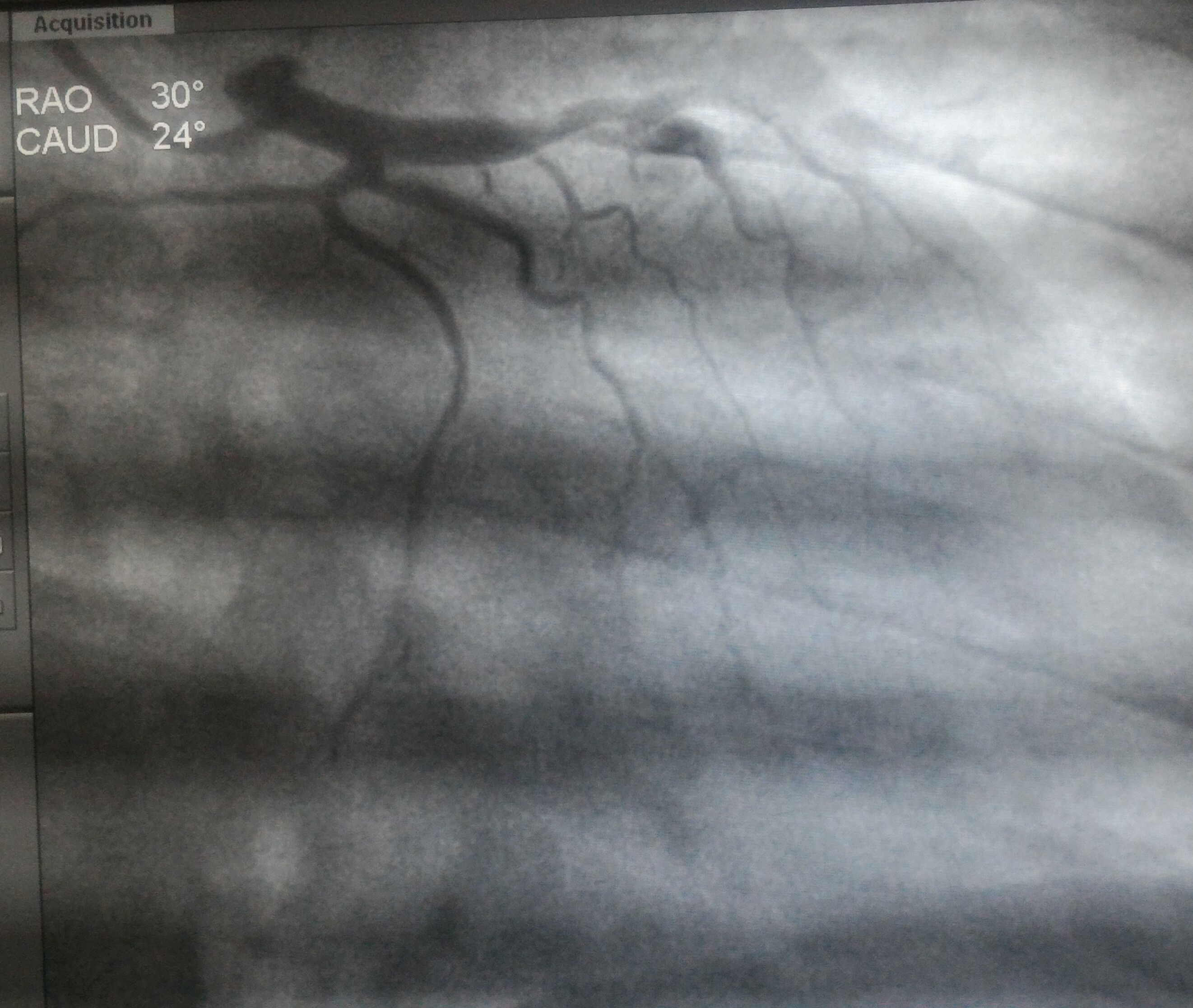
Familiarity with phrenic nerve anatomy is key during an ablation. Specifically, the right phrenic nerve should be carefully delineated during endocardial ablation at key sites, such as SVC, the postero-lateral aspects RA. right superior pulmonary vein, and the junction of the IVC and RA. Fortunately right phrenic nerve never cross over the free wall of RV, unlike the LV,
Left phreic nerve
The left phrenic nerve, on the otherhand, should be localized when performing endocardial ablation near the LAA, ablation of left sided accessory pathways,and epicardial ablation of left ventricular tachycardias
How to avoid phrenic nerve injury during RF ablation ?
There are a variety of ways to displace the phrenic nerve from the ablation site, like fluid, air, or balloon inflation. Here is a step-by-step review article in the Journal of Cardiac Electrophysiology in the current issue, June 2025. It is free access too.
Reference