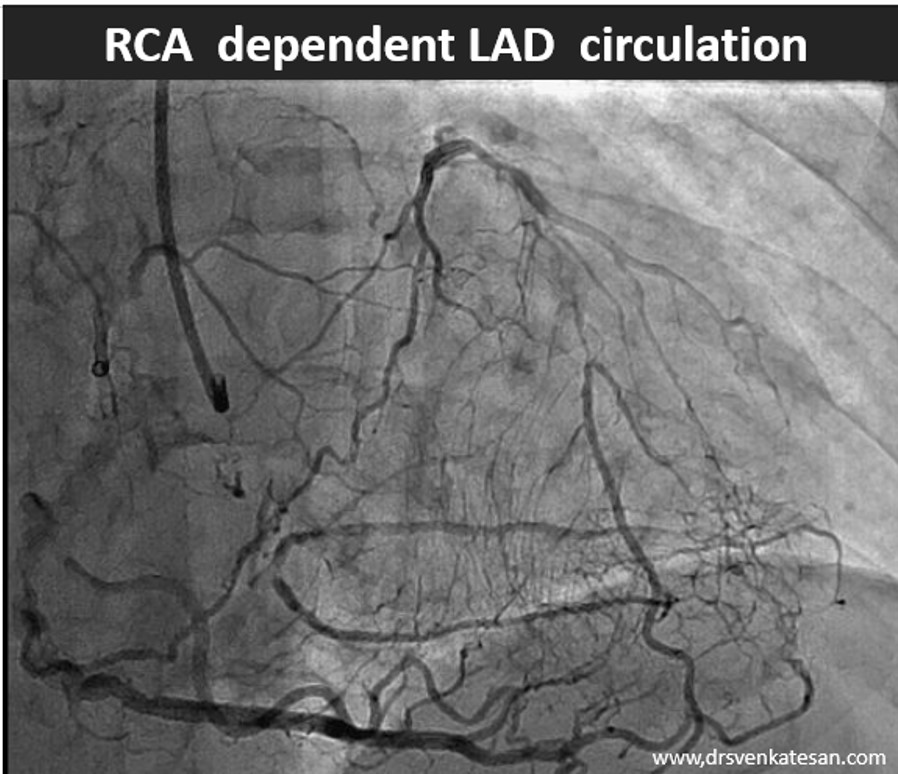
I am sure, this RCA shoot will stretch our coronary acumen
Video source and courtesy: Leizhi Ku,, Xiaojing Ma, From the Departments of Radiology (L.K.) and Echocardiography (X.M.), Wuhan Asia Heart Hospital, Wuhan, China
Did you guess the diagnosis correctly?
It is an acceptable diagnosis, if you thought an anomalous LCA, a LAD CTO or a single coronary artery. But, the true diagnosis is different. It is left main atresia .(Which can also be called a single coronary artery, if RCA gives origin to LCA)
How common are coronary artery anomalies?
It is about 1 to 2%. It can be in the origin, course, and termination. The common ones are the wrong sinus origin. Right arising from the left sinus is much more commoner than left arising from the right. This topic of anomalous origin needs a separate discussion. (Prachi P. Agarwal ,et al Radiographics 2017 )
Left main Atresia: Is it a sub-set of the anomalous origin of LCA from the right sinus ?
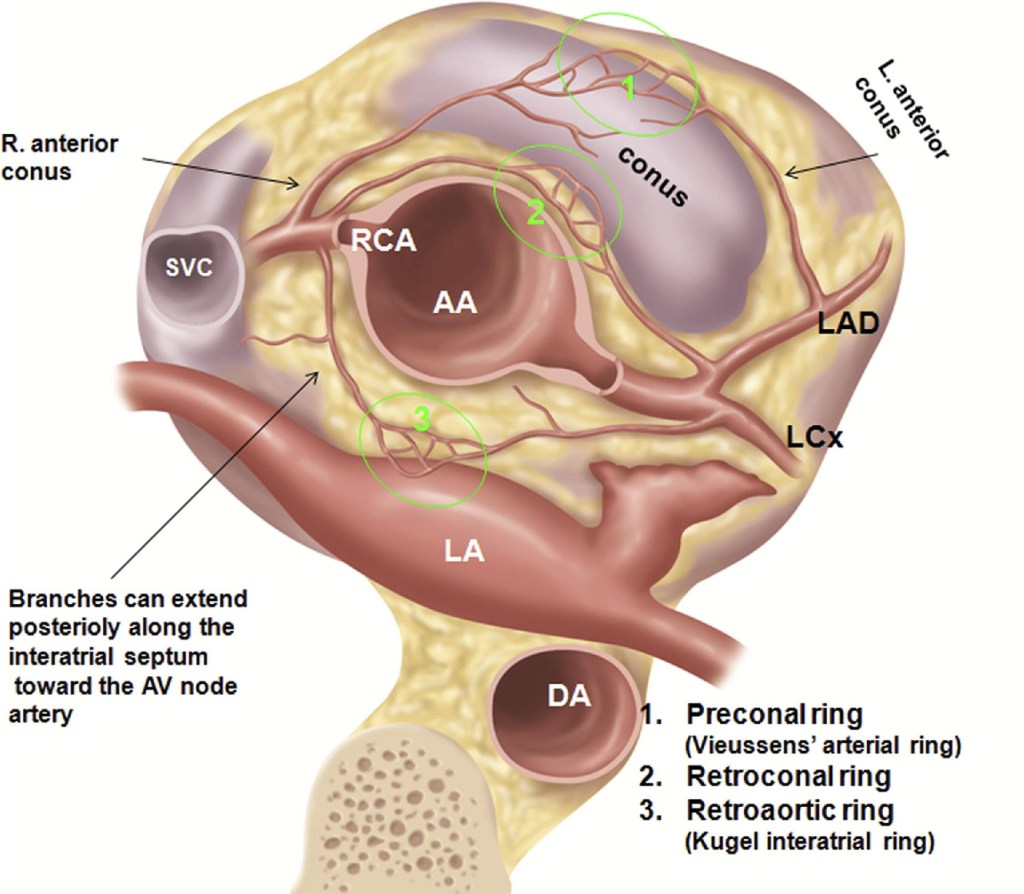
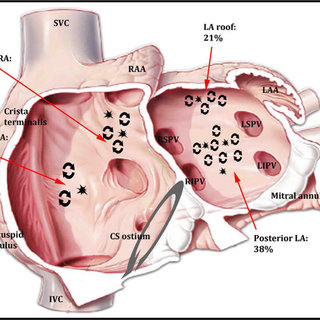
Technically yes, since the left coronary ostium is absent in its designated place in both conditions. But, the entity of true Left main atresia is rare and distinctly different.The difference is, that anomalous LCA often doesn’t travel in the pre-designated path of true LAD and LCX (Ie Intraventricular and Left AV groove). In true atresia, only the origin is sealed. Rest of the LCA is anatomically intact , which gets filled from one of three familiar Inter arterial collateral (Vieussens, Kugel, and retro-conal coronary ring)
Embryological basis of coronary artery anomalies
The left coronary anlagen and bud fail to develop. To know, how and why this happens ( Read here : Sharma B, Chang A, Red-Horse K. Coronary Artery Development: Progenitor Cells and Differentiation Pathways. Annu Rev Physiol. 2017 )
Clinical implication of such coronary anomalies
Apart from angiographic surprises, these anomalous coronary arteries may under-perfuse the ventricle and present as unexplained cardiomyopathy , until we realize the anatomical errors in coronary anatomy.
Some unanswered queries
1. Is the atresia confined to the ostium alone, or does it extend to variable lengths of the left main?
2. How do the fetal and subsequent neonatal LV mass outgrow RV , when the LCA is atretic?
Treatment of left main atresia
Surgery with graft makes logical correction. If absolutely asymptomatic, and the stress test is negative, leaving it, as it is, is not a forbidden option, in spite of the fact, that the patient would have a single coronary arterial supply.
Farhood Saremi Graydon Goodman , Alison Wilcox, J Am Coll Cardiol Img. 2011 Dec, 4 (12) 1320–1323
Acquired mimickers of left main atresia
1. Syphilis
2. Aorto arteritis
3.Ostial Athero-sclerosis( Rare, but status of other areas of coronary artery will usually reveal evidence for atherosclerosis)
True confirmation, is possible only during surgery , ie visulaing the absence of left coronary ostia.
Final message
Coronary arterial anomaly is a less discussed topic nowadays, unless & until, it intrudes an interventional cardiologist in his daily routine life, of delivering stents. In reality, there could be thousands of asymptomatic ones in the public domain. it can result in both risky as well as protective events. One theoretical and realistic possibility can be extrapolated. We know, how adverse is the outcome of Left main STEMI. But, It might also be true in a few lucky souls, one of the above rings can open up instantly and change the destiny.
Reference
- Yassin AS, Dayco J, Kottam A. Left Main Coronary Artery Atresia: Diagnostic
Images of a Rare Coronary Anomaly. Mayo Clin Proc 2023;98(5):655–656. - Musiani A, Cernigliaro C, Sansa M, Maselli D, De Gasperis C. Left main
coronary artery atresia: literature review and therapeutical considerations.
Eur J Cardiothorac Surg 1997;11(3):505–514.