(This is supposed to be a poll. Sorry, readers, you can’t select the answer. WordPress is not kind enough and suddenly made the poll service payable extra. I am already paying nearly a $100 fee to maintain this site. I can’t afford any more.)
We have been taught Bi-Atrial enlargement is the rule in AF .It is still true in most situations. But, we rarely dispute it , & ask which atrium dilates more in AF ?
Let us see few factors.
- Both atria develop from a combination of the primitive atrium, sinus venous, and pulmonary veins.It is logical to presume there must be a hidden morpho-electrical continuity.
- The baseline RA dimension is a few mm more than LA. Further, it is thin-walled, more compliant and can distend depending on volemic status.
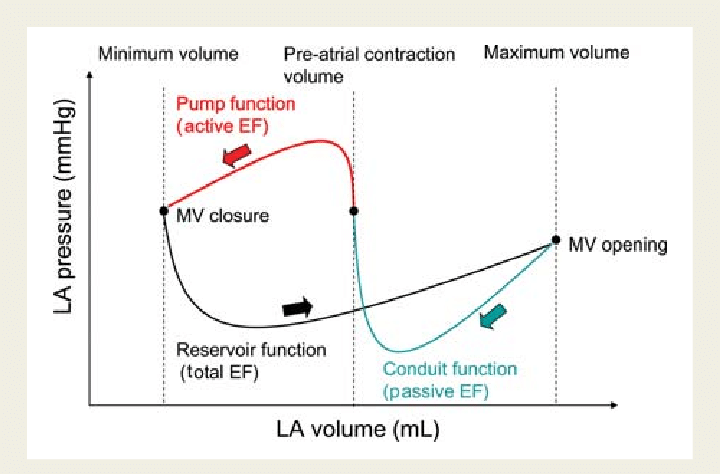
- When atrial fibrillation (AF) begins, it can start with a single focus, degenerating to multiple wavelets, and it spreads throughout the entire surface area of both atria. A fibrillatory wave that occurs at a rate of more than 600 beats per minute can cause fatigue in the long run, leading to atrial dilation.
- In all probability, this dilation is a form of atrial tachycardia and atrial cardiomyopathy. However, underlying lesions such as hypertension, mitral valve disease, COPD, ASD, and TR greatly influence the degree of atrial enlargement.
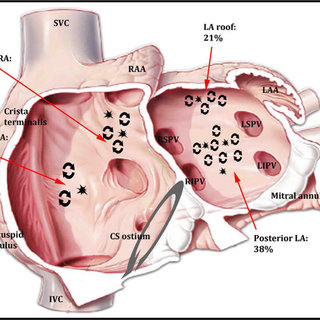
Spatial relationship of sites for atrial fibrillation drivers and atrial tachycardia in patients with both arrhythmias July 2017 International Journal of Cardiology 248(3)
- AF begets AF. This is similar to MR begets MR. Atrial functional MR occurs when the lower part of the atria stretches the mitral annulus. It is important to recall that a small area of the posterior aspect of the LA is a part of the mitral valve apparatus. Therefore, AF begetting MR and MR begetting AF should not be considered a funny rhyme, but rather a realistic possibility.
- Histopathological specimens of atrial tissue in chronic AF can present with surprising results. The atrial muscle can be entirely normal, or the interstitium can be infiltrated with lipids, fibroblasts, amyloid, etc.
- Regarding the issue at hand, it is widely known that in cases of mitral stenosis with AF, the left atrium (LA) is larger than the right atrium (RA) due to the obvious reason that the baseline LA was larger at the onset of AF. However, in cases of lone AF, AF in hypertension, or chronic AF, both atria tend to dilate equally..
Implications for electrophysiologists.
In contrast to other tachycardias, with atrial fibrillation (AF), the focus is often speculative, and ablation attempts are made accordingly. Pulmonary veins have been the primary target for ablation for many years, yet the success rates remain inconsistent. To determine if the AF focus is non-pulmonary venous, such as right atrial, septal, or involving the inferior vena cava (IVC) or superior vena cava (SVC), several techniques are employed to provoke and localize these non-pulmonary vein triggers
Localized atrial fibrosis and interatrial blocks can result in differential fibrillatory counts across the atria. (RA fib-rate can be more than LA, and vice versa.) Is there proof for this, or just an academic gossip? We know atrial flutters can be confined to one atrium. (Pierre Jaïs Circulation 2000) When such flutters transform into fibrillation, how does the spillover of signals occur to the contralateral atrium? On a personal note, we have recorded good E & A Doppler signals across the tricuspid valve, in RHD mitral stenosis, and AF. No published proof as such. I strongly suspect the right atrium can resist the tsunami of approaching fibrillatory waves from engulfing its chamber in at least some patients. An appeal to the new generation EPs who have special flair in AF should look into this and either prove or disprove it.
Final message
My answer to the question is either D or E. Atrial size in AF is not a trivial thing to ignore. This question pushes a simple idea. In primary or lone AF, just by having a look at the RA to LA size ratio, one might get a reasonable guess,about the Initial focus, trigger & pathology of the AF.
A request to all the high profile stake holders involved in the science of PV ablation (either with Ice or fire). Think about all the possible right-sided or septal focuses, before going overzealously for the jugulars of Pulmonary veins, especially if the RA significantly larger than LA . This will save time, effort & of course our reputation.
References
Nil
,