Intra coronary calcium : Are they really pro-thrombogenic ?
A.Yes
B. No ,
C. Yes & No ,
D.Don’t know ?
If you had answered either A or D , you may read further.
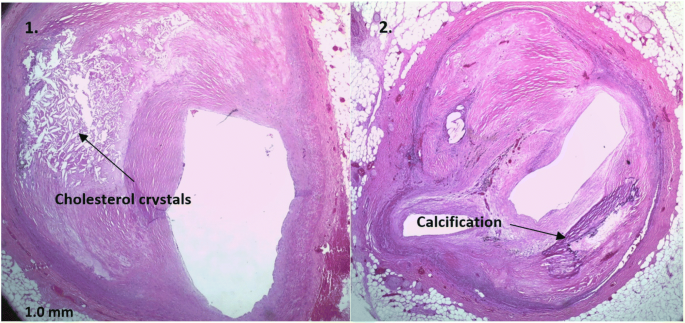
Calcium in the coronary artery is usually in the intimal/medial plane. It is covered by fibrous caps of varying thickness or just a single endothelial layer. Thus, calcium is not exposed to blood directly. Even if it is exposed, as in an eruptive nodule, the formation of thrombus is not attributed to calcium per se but to the exposure of subendothelial tissue factors .
1.If calcium is directly exposed to blood, does it trigger a clot?
Yes is the answer from most of us and even from pathologists. But the proof is vague. If that is the case, every degenerative, calcific aortic or mitral valves must form recurrent thrombosis. Thrombosis over these calcification are very rare , with 7500 liters blood traverse over it every day. (Now you know, why your answer was wrong)
2.Is it not true, calcium is essential in the clot forming process ?
Yes, Calcium is essential for the blood coagulation process. It is required for several key steps in both the intrinsic and extrinsic pathways, acting as a cofactor for the activation of various clotting factors.
Please mind, this free calcium is totally different . They are ionized calcium circulating in the blood , always charged to bind with a clotting factor.
3.Then how calcium is not pro thrombotic ?
Read below
4. Is the calcium in the blood and deposited Calcium Different?
Absolutely. The calcium that takes part in the coagulation process is free ionic calcium. Deposited calcium, within arterial plaques, valvular calcifications, is fundamentally different. It exists primarily as insoluble crystalline compounds, such as hydroxyapatite (a form of calcium phosphate) which is the same mineral found in bone. This is a solid, bound form resulting from dystrophic or metastatic calcification process. The are largely Bio -Inert atleast with reference to coagulation.
Final message :
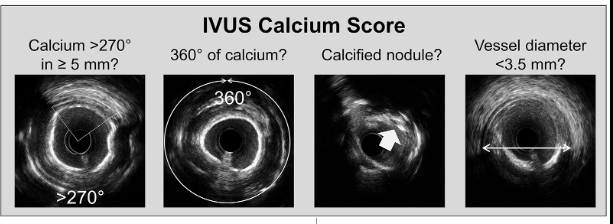
Coronary calcium, whether within the tissue plane or exposed to the lumen, is not directly thrombogenic. They are dead-end inert products of atherosclerosis. However, the prothrombotic trigger occurs with some of the sharp calcium crystals or nodules when they injure the endothelium and expose the subendothelial tissue factors. Abluminal endothelial injury from the intimal calcium is far less common* in most chronic CAD, unless , some aggressive humans decide to wage a intra-coronary calcium warfare, to facilitate stent deployment .
*Disproportionate calcium loading in the shoulder region of the plaque can make a plaque vulnerable. Having said that, overall in a holistic atherosclerotic landscape, calcium is more of an enemy of cardiologists, who face a hurdle to place stents than the patient who harbor it..