There is no simple answer. We hide behind two terms, adaptive and maladaptive RVH. While the former is beneficial for an unknown period of time, the latter rapidly goes into a downward spiral.
- Adaptive RVH (A-RVH) occurs when the RV responds to chronic pressure overload by increasing muscle mass concentrically. This adaptation maintains RV contractility and cardiac output despite increased pulmonary vascular resistance. RVH is typically concentric with less chamber dilation, preserved coronary perfusion,
- Mal-adoptive RVH (M-RVH)occurs If afterload is excessive, prolonged and the RV cannot maintain sufficient contractile function . For some unknown reason, in M-RVH, the impact of PA pressure is not uniform the chamber dilates asymmetrically this leads to wall stress increase, fibrosis, ischemia, and contractile failure.
I am unable to find the exact incidence of the above two entities. In COPD, it is more adaptive; in cardiac conditions, it is more maladaptive. A new thinking is that the LV plays a significant role in determining RV function, as both are interdependent. (Both arms of Bernheim effect)
The third entity is acute RV dilatation to sudden elevation of PA pressure as in PE. (Recall the 60/60 sign) Though we think it is purely a hemodynamic response, there are reasons to believe an ultra-rapid predetermined genetic response is also possible by recruiting messenger RNA and growth factors.
*It is worthwhile to note the complexity of RV dynamics. Chronic RV dilatation, (without pressure load)need not be a major pathology, as they are meant to dilate with excess venous return (We also see ASD patients live their entire lives with baggy right ventricles.)
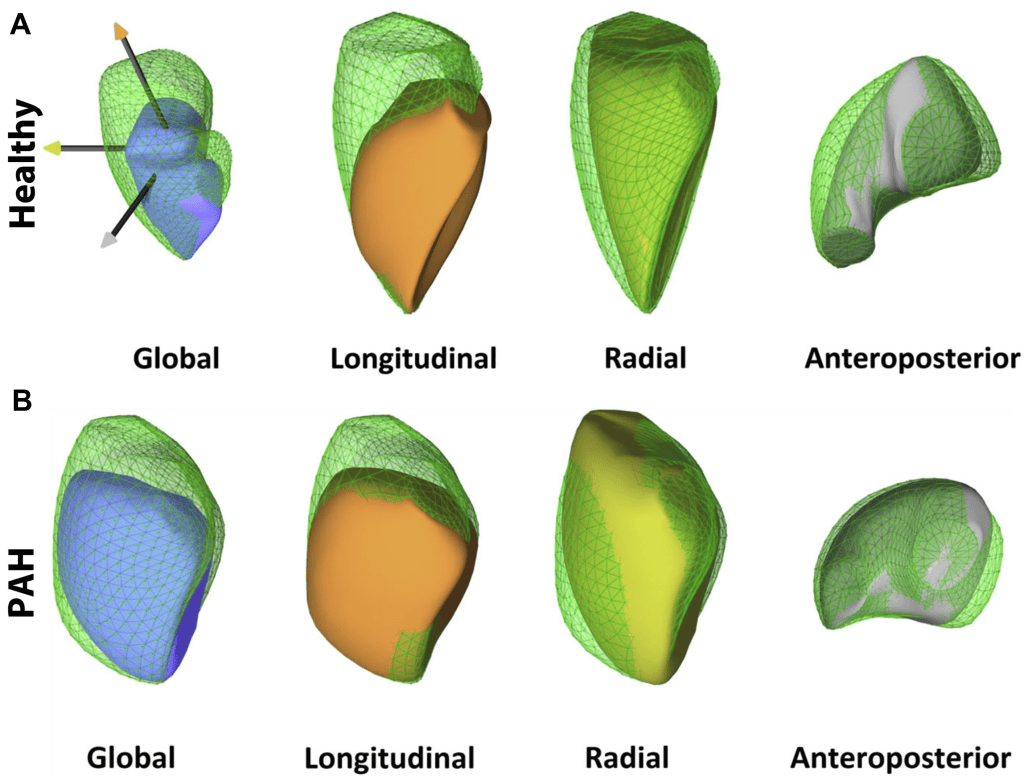
Various shapes of RV in PH .Image source : Llucià-Valldeperas A, de Man FS, Bogaard HJ. Adaptation and Maladaptation of the Right Ventricle in Pulmonary Vascular Diseases. Clin Chest Med. 2021 Mar;42(1):179-194.
Mechansims of adoptive RVH
The following mechanisms are believed to be responsible.
- Concentric hypertrophy with preserved contractile function involving mainly fast myosin heavy chain (MHC) α isoform expression.
- Metabolic remodeling with a switch to glycolytic metabolism but preserved energy supply through compensatory mechanisms like increased GLUT-1 expression.
- Maintenance of angiogenesis and oxygen supply through vascular endothelial growth factor (VEGF) signaling.
- Self restricting fibrosis and balanced extracellular matrix remodeling.
Is there any Clinical and echocardiographic clues to adoptive RVH ?
Of course yes. But all are common sense related.
- Patients with adaptive RVH often maintain higher exercise tolerance.
- Elevated levels of BNP or NT-proBNP correlate with maladaptive RVH.
- In echocardiography , Adoptive RVH is characterized by increased RV wall thickness (>5 mm) with relatively preserved RV chamber size and function. TR is less common as shape is preserved and annular distortion is minimal.
How long the Adoptive RVH phase can lasts ?
Law of Laplace states, wall thickness will reduce the after-load, balance out the RV-PA coupling mis match. How long this can last? A wild guess is that it can last even up to a decade. Studies in conditions like surgically repaired congenital heart disease and Eisenmenger syndrome have shown adaptive RVH with preserved contractility and normal chamber size for many years. However, this phase eventually transits to maladaptive state.
Can we Induce adaptive RVH as a therapeutic measure ?
As of now , this possible only on paper .Research should target therapeutically, controlled pressure overload and neurohormonal modulation can promote beneficial RV hypertrophy. Strategies to support favorable metabolic pathways, enhance angiogenesis, and reduce oxidative stress are under investigation
Final message
Whether the RV is going to fight or flight the raising afterload of pulmonary HT is not in our hands. It is pre-programmed and switches are controlled by destiny. We can only do whatever, to lower the PA pressure and PVR by treating the primary cause if any. Though, the pharmacological strategies in PH has shown tremendous progress in recent times , the behavior of RV will define the outcome.
Reference
Post-amble : How the new age interventions help tackle the RV failure
TR clips, and tricuspid valve reconstruction, either surgical or percutaneous, RV assist devices are THE interventions done in a failing RV before the last resort of heart/Lung transplantation.



