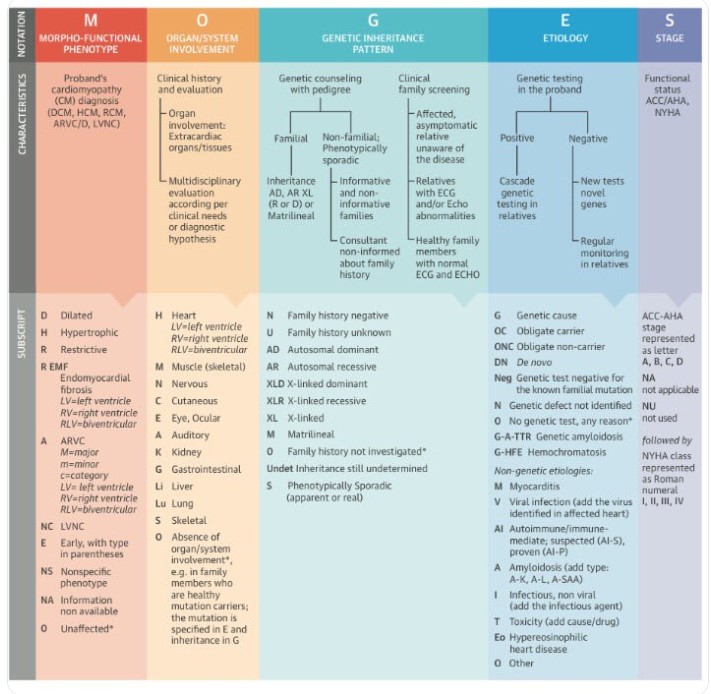
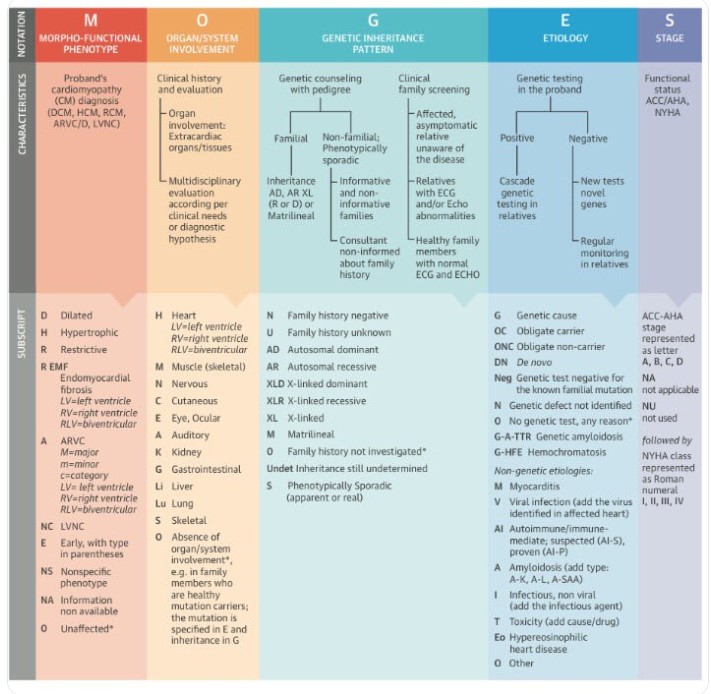
The term Ischemic cardiomyopathy(ICM) was originally coined by Dr. Burch from Tulane University, New Orleans, USA in 1970. For many decades there was skepticism regarding the existence of such entity. WHO classification over the years never included this term. ESC working group of 2008 (Elliott P, European Heart 29(2):270–276) decided not to include CAD as a cause for cardiomyopathy. Even the current MOGES system doesn’t invoke CAD as a cause for cardiomyopathy. But, I am sure, most of practicing cardiologists would agree, there is a need for such an entity.
Why there is much reluctance to diagnose Ischemic cardiomyopathy as a distinct entity?
It is because of the basic principle, that cardiomyopathy should be a primary disease of cardiac muscle. (or at least secondary ).The presumption is, Ischemia per se doesn’t lead to muscle disease as such. It is just nutrition deprival.
Does this justify?
No, not at all. When a cardiac muscle is chronically deprived of nutrients it goes for necrosis, dilatation, scarring and dilatation, and progressive LV dysfunction. At some stage, it becomes true muscle disease or its equivalent (Secondary cardiomyopathy).In fact, adverse remodeling, Infarct expansion, extension lead to myocyte disarray, slippage and apoptosis, and cellular and interstitial fibrosis. All these changes are similar to Idiopathic (Postmyocarditis)cardiomyopathy.
What happens in the real world?
Even though there was some hesitation to diagnose ICM in the past, gradually the term shrugged of its taboo in academic circles. In heart failure clinics the only question seems to matter for everyone is, Is it Ischemic or non-ischemic DCM? Surgeons and EP guys also actively pursued the term Ischemic cardiomyopathy while they are selecting patients for CABG or CRT/ICD etc.
Further, in the research world involving community-based heart failure cohort, they required a basic distinction between the group of Ischemic from Non-Ischemic cardiac failures.
DUKE university definition (By Felker et al)
I think DUKE ended the controversy in the Nomenclature of Ischemic cardiomyopathy. It suggested the following to diagnose ICM (Read REF 2)
- LV dysfunction < 40% EF
- >Atleast one significant proximal coronary lesion (Usually 2 or more)
- With the history of MI or Revascularisation
* We are analyzing our data (Madras medical college, Chennai India) and propose to write WHO/WHF to include the following additional criteria to diagnose ICM.
4. At least 6 months should be elapsed between the MI and diagnosing Ischemic cardiomyopathy,
5. Must have significant LV dilatation & global Hypokinesia(With or without regional variation).
6. At least one episode of clinical heart failure is required before labeling it as Ischemic cardiomyopathy.
Other definitions that endorsed Duke
STITCH criteria *Surgical therapy in ischemic DCM study ICM was defined CAD with cut off EF < 35% with triple or double vessel disease.
iFAQs in Ischemic cardiomyopathy
1. Can we diagnose ICM without a history of MI?
This is tricky. As we all aware its very much possible as in silent MI of diabetes. One more possibility is even chronic coronary syndrome with microvascular dysfunction can lead to ICM.
2. Can Ischemic cardiomyopathy present as HFpEF or RCM?
While most Ischemic Cardiomyopathy present as DCMs with HFrEF, It is currently not clear how much of Ischemic heart failure present as HFpEF and if so they can’t be included technically as Ischemic cardiomyopathy in spite of the fact they present as HF.(as EF would be >50%)
3.When does a Post MI failure become Ischemic cardiomyopathy?
If the definition of STITCH or DUKE is applied, any acute STEMI can fulfill criteria of ICM. Hence it advisable to have a time limit say 6 months following MI to be referred to as Ischemic DCM. Pathologically to call it true cardiomyopathy, scarring, dilatation is required. Myocytes should be in independent self-destruction mode irrespective if hemodynamic conditions.
Response to treatment
The only purpose to diagnose ICM is to try to remove the I from ICM( ie Ischemia) Unfortunately, it is not an easy task. (While correcting Ischemia in ACS seems to be such an easy job.)
Following principles apply.
- Medical management of HF/Ischemia is the key.
- It is advisable every patient with cardiomyopathy should undergo coronary angiogram to rule out ICM.
- Effect of revascularisation remains equivocal.
- Viability of remaining muscle mass must be documented. (At least one-third of total cardiac mass should be viable.(Not very easy to prove though)One may use Doubutamine /Nuclear stress/PET etc) .It’s very important to realize even if the viability is demonstrated, the area that shows viability must be supplied by an artery that has a revascularisation eligible lesion.
- STITCH can be called as a negative study (meaning positive outcome for patients if the patient doesn’t receive CABG in mulitvessel CAD and LV dysfunction ).However , STICHES (Extension of stich showed some long term benefits) The probable reason for CABG not helping much in ICM is the muscles didn’t get further useful life, either because it’s fully dead or extremely viable, that revascularisation made no impact.
- CRT/ICD is known to prevent SCD and improve the functional class.
- Heart transplantation is a life-modifying specific strategy.
Final message
I agree, many times our valuable time is wasted in renaming /Altering /relabeling a disease /process or pathology without any useful purpose. Medical nomenclature and classifications are done to make diagnosis simpler, choose an appropriate therapeutic modality and make a positive impact on the outcome.
In that sense, segregating ICM from other causes of cardiac failure do help in choosing a specific management strategy.
Let us welcome MOGES, It is the most comprehensive cardiomyopathy classification system (Like TNM classification for cancer). Still, I am not clear why it hasn’t included CAD in that system. Thanks to Dr. Burch who thought of this 50years ago.
Reference
1.Burch, G. E., Giles, T. D., & Colcolough, H. L. (1970). Ischemic cardiomyopathy. American Heart Journal, 79(3), 291–292.
2.Felker G.M, Shaw L.K, O’Connor C.M (2002) A standardized definition of ischemic cardiomyopathy for use in clinical research. J Am Coll Cardiol 39:210–218
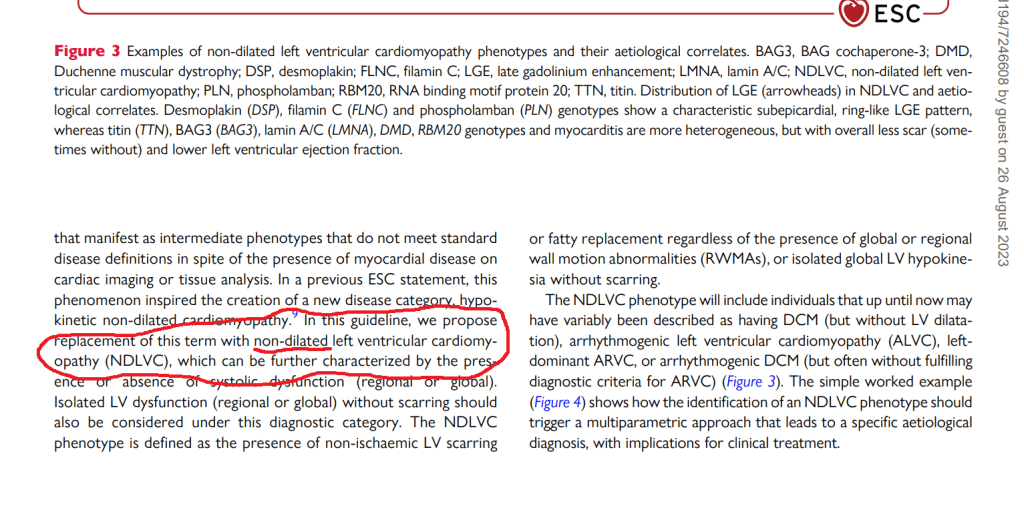
History of cardiomyopathy classification
The landmark thoughts originated in 1972 .When Goodwin and Oakley defined cardiomyopathies as the heart muscle diseases of unknown cause and described them as dilated (DCM), hypertrophic (HCM), and restrictive (or obliterative) (RCM) cardiomyopathy types.
WHO adopted it mostly and suggested Primary and Secondary cardiomyopathy in 1980. In 1995 WHO revised it.
The current MOGES classification doesn’t mention about Ischemic etiology
Read Full Post »