Once upon a time, long, long ago, cardiologists used to be worried about akinetic segments, scars, dead tissue, and Q waves before attempting revascularization by either PCI or CABG. Now, the concept of myocardial viability has become a cliché ( rather demeaning) at least within the cath labs. Currently ,we follow a self administered whip . Every post-MI patient should be considered for revascularization as a default strategy irrespective of the level of dysfunction or scarring .This can happen either in the IRA territory or non-IRA territory or both.
This strategy is now dis-armed with fresh evidence in the form of REVIVE -BRICS trial. However, there could be some distinct errors in the way many Interpreted this study. (Read here about REVIVE tral Perera D, Ryan et al JAMA Cardiol. 2023). One reason viability testing lost its sheen is the fact, identifying the extent of viablity requires a complex battery of tests. If we have simple clues on bed side, the adoptation of this concept would not have become a challenge.
Lets go back and learn something from the year 1999
For those cardiologists who believe myocardial viability is still an important factor before revascularization, let me pull out a 30 year-old study from the University of Aberdeen, UK, that looked into the humble ECG to detect viability. The authors went beyond just observing presence or absence of Q waves .It conveys a great learning point.
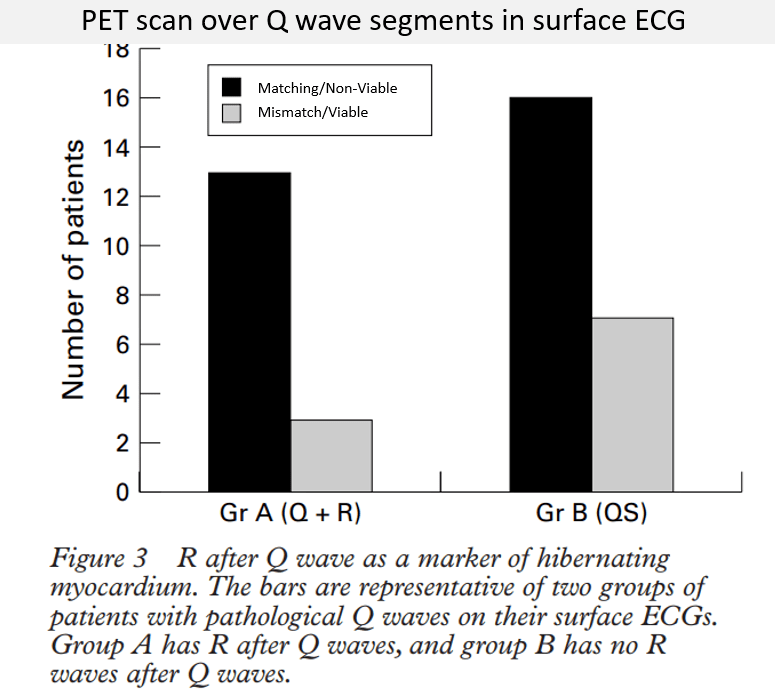
Modified from Al-Mohammad A, et al Heart. 1999 Dec;82(6):663-7. (Ref 1) Matching means non-viable myocardium (Tissue looks akinetic or scar-like, while PET concurs and shows lack of metabolic activity. This is referred to as matching, and the segment is non-viable) Mismatch means viable myocardium (Tissue appear dead by akinetic Echo but metabolism intact ie a mismatch implying viability )
It is worthy to note, the authors looked specifically over the segments that subtended Q waves and looked for viability matching. It was correlated with a PET scan, the gold standard for viability testing even now.
The results were important and insightful. What we infer from this study is actually a simple message. In post-MI patients, even with the burden of q-waves, if the return wave overshoots the baseline and inscribes some sort of r-wave (Qr, QR, qR patterns), there is a high possibility of viable tissue when compared to QS wave. It is a new lesson from a old paper for me. , ie any R is good whether it is preceded by q or not.
It is good to recall ,other simple clues to the presence of viable myocardial tissue, such as presence of angina, M-mode wall thickening. Not to forget other modalities like, well preserved sub endocardial function by speckle tracking echo, dobutamine-stress, myocardial contrast echo, and LGE-MRI.
Final message
As on 2024, the concept of myocardial viability testing has not vanished. We must ensure, not to pass on a incorrect message to generation next cardiologists, that viability tests are outdated and obsolete.
Reference




