None exposes the expertise and stretches the electrophysiological acumen of a cardiologist, more than a strip of wide QRS tachycardia. Here is a patient who comes with palpitations, with mild hypotension , still comfortably entering the OPD with a non-emergency appointment.
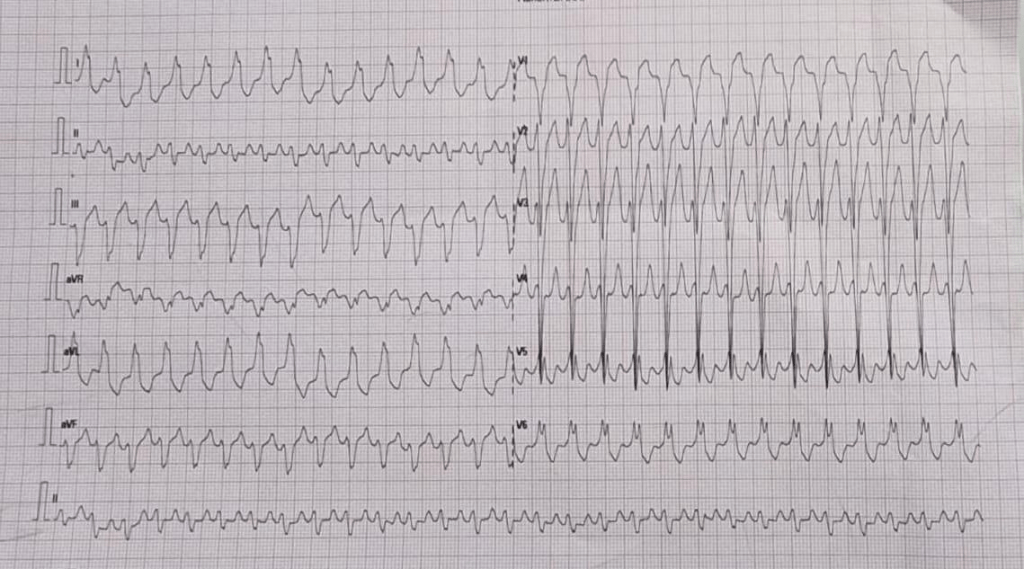
How many diagnosis are running through your mind when you see this ECG . How much it got narrowed after applying criteria like Brugada, Vereckei etc ( VT, FT, OTVT, Mahaim Tachycardia, AVRT /AVNRT with aberrancy etc)
Now let me reveal the age of the patient .He is a 13 year old boy. Does this help you to narrow down the list of possibilities ? Logically, It should , but for some it can widen the list as well .( Brugada, Anderson, Long QT, Naxos all runs through the mind)
What happed next ?
As the cardiologist was wondering how to tackle this arrhythmia . Adenosine? Amiodarone or DC shock, thankfully, the boy got to spontaneous sinus rhythm .
Click here to see the ECG after restored sinus rhythm & the diagnosis is Instant .
Yes it is a WPW substrate. Localization of pathway is a must and a headache for the fellows. .For me, It looks like a posterior pathway in the para-spetal area. 90% of AVRT are narrow QRS . Here it is wide. Why ?
It’s simple. The tachycardia is anti-dromic.
Is it ? Look at the strip again and confirm is this antidromic ?
I am not sure , I still think it is still antidromic .
I am saying No. This is Ortho-dromic wide QRS tachycardia .
How do you say so ?
Antidromic will still more wide and rapid and won’t terminate spontaneously .Of course one problem here aberrancy usually take an RBBB morphology.
How are you so sure . Let us send this to an EP guy.
*What did the EP say? Well, he didn’t commit to anything as I expected. He said until he measures the refractory period of the accessory path, he won’t comment anything about ortho or antidromic query of AVRT. He asked us to send the case for ablation immediately,
Ok. Let us analyse the reason for orthodromic wide QRS AVRT
1.Rate dependent aberrancy
2.Functional abberancy.
3.Preexisting BBB
4.If patients are on drugs that can prolong his Purkinje conduction
Final message
Two lessons may be learnt.
Lesson 1: Trying to decode a wide QRS tachycardia, without knowing clinical background, should be forbidden. This topic is intentionally made complicated by a flawed teaching methodology of wide QRS tachycardia for over 4 decades. Maybe the single lead AVR algorithm promises to be a quick remedy. If AVR is positive, it is VT; cannot be SVT.
(For the curious readers , please go through Dr. Masood Akhtar’s article from Wisconsin on how to differentiate VT & SVT without even looking at the ECG by law of statistics that beat the invasive EP studies).
Lesson 2 : Wide QRS AVRT is not always antidromic . In fact, orthodromic wide QRS AVRT is 2 to 3 times more common. Many of us don’t realise this bias in our learning.
Related topic
How common is orthodromic wide QRS atrial fibrillation ?
Reference
Acknowledgemt
The ECG is posted with courtesy of my colleague Dr. C.Moorthy, Cardiologist, Chennai.

