We presume ECG fails miserably against echocardiography for assessing hemodynamics , while echocardiogram has little value when it comes to studying electrophysiology . Ironically , we often ignore the fact , ECG can provide important long-term hemodynamic data . The pattern of chamber enlargement give us vital clues to the prevailing hemodynamic stress and loading conditions. While echo can be termed as an anatomical and physiologic modality , ECG apart from its unique capacity to record cardiac electrical finger prints , it provides useful , anatomical , hemodynamic information too !
While Doppler is a fascinating modality to measure hemodynamic data in a moment to moment fashion it can never ever tell us , what has been going around in the preceding months or years. This is were chamber size helps which give us chronic physiological information (Chronic Doppler ?)
A simple E:A reversal in mitral inflow doppler can be a innocuous finding in isolation . If it is associated with even minimal grades of LAE it gains huge importance. That is why left atrial size is funnily referred to as HB A1C of diastolic dysfunction ( A marker of chronicity of diastolic dysfunction)
If LAE is so important to diagnose diastolic dysfunction , why we are so obsessed with doppler filling profiles of mitral valve ,pulmonary veins, mitral annular tissue Doppler and what not ! .Many of these sophisticated doppler methods are extremely operator dependent and are subjected to technical and mathematical errors. Especially , with tissue doppler where we magnify the errors as we filter extremely slow tissue motion .
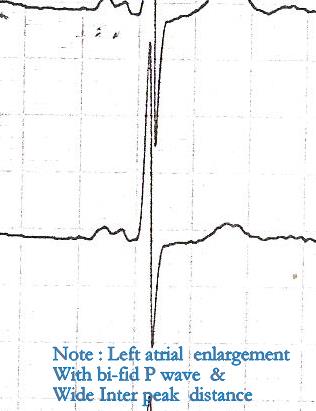
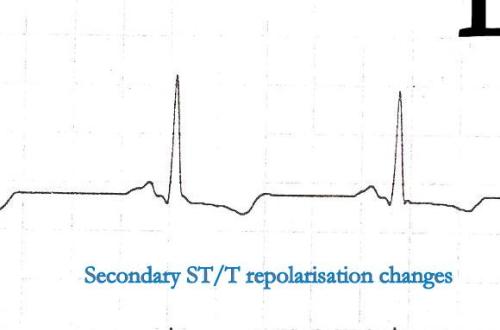
For many decades we have failed to impress ourselves , about the importance of subtle P wave abnormalities in the ECGs of hypertensive patients.
In fact those innocuous looking slurs and notches in P waves , suggest the left atrial stress and a definite marker of underlying LV diastolic dysfunction .
P wave is the only electrical wave that occur in diastole .Hence there is no surprise ,i gives us enormous information about this phase of cardiac cycle .
If only we look at them carefully, zoom it (Now it is made easy with so many softwares) analyse critically we can find a wealth of information about the atrial behavior in hypertension.
Experience from our hypertension clinic with periodic echocardiograms suggest , the following ECG findings can be good markers of significant diastolic dysfunction .
- Notched P wave
- Wide P waves
- Slurred P wave
- Bi-phasic P waves
* Surprisingly , these abnormalities correlated with at least grade 1 diastolic dysfunction even in the absence of for LAE or LVH by echocardiogram.
** In an occasional patient P waves can widen due to inter atrial block or conduction delay. This a rare exception for wide P waves without LAE.
Final message
A well recorded and analysed ECG can predict diastolic dysfunction with fair degree of accuracy .This fact need to be emphasized by every one . Next to ECG , LA size and volume by 2d echo are excellent parameters to assess diastolic function in a long term fashion. Sophisticated but error prone , momentary doppler parameters are getting too much attention at the cost of simple , shrewd ECG and 2D echo !