Archive for November, 2025
What is the realistic definition for “fact vs fake” news
Posted in Uncategorized, tagged bmj, dr s venkatesan, expressions in cardiology, fake vs fact in medical science, jama network, lancet, madras medical college, medical education, medical ethics, nejm, quotes in medical ethics, venkatesan sangareddi on November 18, 2025|
Does IVS hypertrophy occur in Pulmonary hypertension ?
Posted in Uncategorized, tagged D shaped IVS and septal thickness, D shaped septum in pulmonary hypertension, IVS thickness in pulmonary hypertension, RV free wall thickness vs IVS thickness in RVH, RVH in pulmonary hypertension, Ventricualr interdependence on November 18, 2025|
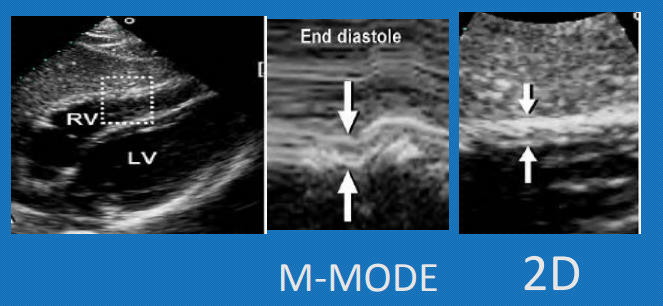
Interventricular septum, is the common shared wall between LV and RV . For various biological and hemodynamic reasons , this sharing never follows the law of equity.. It has a bias toward the bigger brother LV. Still, it never lets the RV down in contributing to RV function.
Let us see, how the IVS behaves when it comes to responding, to RV pressure overload .It is clear ,from what we know so far, IVS behavior rarely follows a pattern. We know it resists the pressure and transforms to a D shape. Does the D shaped LV really trigger an increased IVS thickness ?
IVS hypertrophy in RVH : A mixed mystery pheonmenon
In pulmonary hypertension (PHT) or any right ventricular hypertrophy (RVH), the interventricular septum (IVS) does not hypertrophy primarily due to its unique hemodynamic positioning, as IVS is anatomically and functionally linked with left ventricular (LV) mechanics. Unlike LV, the chronic RV pressure overload which is required for septal myocyte growth is rarely sustained because RV tends to dilate as well, in the process interrupting hypertrophy.
RVH occurs with elevated pulmonary artery pressures , but the pressure distibution is uneven. It is more on RV free wall and outflow tract rather than the septum. The pressure distribution concentrated at the RV free wall (infundibulum and body) .Also, the trabeculae sparing effect on IVS from direct overload .
RV free wall hypertrophy defined as thickness exceeding 5 mm on echo in subcostal view in end diastole, ideally on inspiratory phase when it is maximally filled. ( MRI is a still more reliable index of RVH severity) correlating well with RV function and prognosis.
Final message
IVS rarely hypertrophies in RVH in most pathological RV pressure overload conditions. This is due to the complex shape of the RV as well as the non-uniform pressure distribution of RV intracavitary pressure. Unlike LVH, there is no strict concentric RVH. RV free wall hypertrophy is the best index for accurate identification and quantification of RVH.
A note of caution
Congenital heart diseases like isolated valvular PS, TOF can cause severe IVS hypertrophy. Similarly some Inherited or acquired infiltrative diseases can cause disproportionate RVH .We should be cautious , not to mis-classify IVS hypertrophy as LV pathology in these situations.
Reference
In HFpEF , which chamber of the heart primarily fails ?
Posted in Uncategorized on November 14, 2025|
A. Left ventricle
B. Left atrium in isolation
C. Both left ventricle & left atrium
D. Isolated right ventricle failure.
E. It is actually a Bi-Ventricular failure.
Trying to answer
If any one can answer this question, correctly , he deserves some award. I am yet to find an answer.
HFpEF , by its definition has Normal EF, diastolic LV failure , LA reservoir dysfunction, combined post and pre cap PHT, with or without RV failure.
Full blown HFpEF has some what curious hemodynmics. Though we expect LA to fail in isolatiin, it is the right ventricle, that over works to tackle the elevated LAP and PH . Hence, it is likely clinical RV failure would be more common than LV.
Therorticaly, we can say , HFpEF is typical example of Bi ventricular failure as well, ie LV diastolic ,and RV systolic failure. If you want to be still more precise, it should be called triple chamber failure (LV,LA & RV)
Final message.
HFpEF continues to be complex clinical entity, with no single chamber is a primary culprit. It is a multi chamber failure. In fact, the failure initiating chamber may play lesser role than the responding chamber may react disproportionately. Please Note : LA is failure defining chamber. If it can tackle the stiff LV with all its might (compliance and contractility) , no other chamber need to fail.
Knowing the Heart diseases, with female pre-ponderance
Posted in Uncategorized, tagged female heart disease, gender difference in women with heart disease, gender ratio in heart disease, heart disease with female preponderance, takayasu arteriits, why rhd affects more women ?, women centric heart disease, women with heart disease on November 13, 2025|
Men are from Mars, women are from Venus. It may not be a fiction.afterall .It runs deep into q-bits and quark particles of our cells. The well known double X cross chromosome, epigenetics , along with hormonal interactions with cellular components make many of diseases more female centric.
Most importantly, women who are carrying a baby , are technically a chimera, and the two-way traffic of genetic materials across the placenta has unexplainable Immune interactions, making autoimmunity almost exclusively a female disorder (SLE, etc.).
Following is the partial list of women-centric heart disease
- Rheumatic Heart disease: RHD is common in both genders, but it attacks the mitral valve with a strikingly different rate in females, with a ratio of up to 4:1. This difference, however, wanes with aortic valve involvement.
- Mitral valve prolapse: More common in women, overriding the the fact, there are more tall men , who are likely to have more MVPS
- Takotsubo (stress) cardiomyopathy: 80-90% casesoccur in women. This is surprising. (Women are known to be great fighters of stress, in all walks of life; they outlive men by 5-10 years in terms of longevity. Still, when it comes to the heart, they seem to be sensitive.)
- NSTEMI vs STEMI in women (It is rather women are somewhat resistant to STEMI )
- Sponatneous coronary artery dissection has well known female domnace especailluy in duiring pregnancy (estrogenic vascular elastin fracture , striae gravidourm ?)
- Coronary microvascular disease: Higher prevalence in women; female rate up to 66%
- Peripartum cardiomyopathy: Exclusive to women by definition, incidence 1 in 5000 live births
- Heart failure with preserved ejection fraction (HFpEF): Women represent about 55-60% of cases. Odds are higher for sure. (Is that obesity ?)
- Primary pulmonary hypertension (Pre -capillary , again hormonal-endothelial interaction ?)
- Takayasu arteritis (aorto-arteritis): Strikingly high. Female to male ratio approximately 7:1
- Mitral annular calcification: Female to male ratio roughly 2:1; more severe in women, especially elderly (Aortic annulus , males dominate )
- In congenital heart disease Atrial septal defect has a female to male ratio approximately 2:1 (To remind TGA is strikingly a male disease)
Missing entities , may be added by readers
Final message
Knowing the gender difference in heart disease may not matter much, if we look at things superficially. Decades down the line, It has a huge potential in preventive cardiology, as the current genome-level interventions and female-specific vaccines might be in the offing.
References
- .Gewitz MH, Baltimore RS, Tani LY, Council on Cardiovascular Disease in the Young. Revision of the Jones Criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography: a scientific statement from the American Heart Association. Circulation. 2015 May 19;131(20):1806-18.
- Templin C, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373(10):929-38.
- Lanza GA, Crea F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation. 2010 Jun 1;121(21):2317-25.
- Nishimura RA, et al. Mitral Valve Prolapse. N Engl J Med. 2007;356(26):2641-9.
- Sliwa K, et al. Peripartum Cardiomyopathy. Circulation. 2010;121(8):840-50.
- Dunlay SM, et al. Heart Failure with Preserved Ejection Fraction: Drivers and Therapies. JACC. 2017;69(17):1919-1932.
- Johnston SL, Lock RJ, Gompels MM. Takayasu arteritis: a review. J Clin Pathol. 2002;55(7):481-6.
- Abramowitz Y, et al. Mitral Annular Calcification. J Am Coll Cardiol. 2015;66(17):1934-41.
- Warnes CA. Adult congenital heart disease: Specific considerations for women. J Am Coll Cardiol. 2016;68(7):747-760.
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39(12):1890-900.
Forbidden quotes in the Principles of practice of medicine
Posted in Uncategorized on November 11, 2025|
News: 80% of investigations Doctors do, every day is done to satisfy, the self, the science, the patients , the peers & the hospitals or just to label a symptom complex into a disease.Just 20% help us in arrive at a diagnosis. The Irony is, it is not dificult to seperate these two categories. In fact, most of us are very much aware of junk component.
Further bit of a news : 90% of global cost of medicine is spent in prolonging the final 30 days of life of our beloved patients.

Final message
When we enter the medical school as young doctors we were taught that “Principles of practice of medicine dictates , we should always strive hard ,every moment, for an accurate diagnosis before we start the treatment for our patients” Now , after four decades into the profession , something is haunting, and trying to un-do this foundational lesson in medicine.
Post-amble
What a nonsense statement ? Do you want the modern medicine to go back to medieval times?
“Indication & timing” of PCI in STEMI with multivessel CAD : RCTs are the true culprits !
Posted in Uncategorized, tagged timing of pci in multivessel pci on November 9, 2025|
One of the intensively discussed, but casually taken concepts among the interventional cardiology community is to decide, when to do PCI in a non-culprit vessel in STEMI ? It is more of desire driven, rather than data driven Interventions. ( To fulfill the grandeur- mirage of complete revascularization , which occurs only in lab models )
Evidence pendulum (Ref below : MULTISTARS-BIOVASC-FIRE -COMPLETE–CULPRIT SHOCK)
The pendulum is swinging continuously from immediate multi-vessel PCI to delayed, deferred, (how much or as you like?) The problem is. these pendulums can be set into motion, as we desire , by different stake holders and publish them too in major journals like NEJM, Lancet, etc. The COMPLETE-NESS of evidence is mostly In-complete, if we scrutinse it properly.
Prolonging our playtime in an ACS ridden coronary artery, with a multivessel PCI can be really problematic. Every experienced cardiologist knows this fact. But RCTs (& some peer groups) that come from nowhere confuse them. Of course, some RCTs do give us the right lead. It is very unfortunate that many of us failed to learn an important lesson from the most remarkable trial CULPRIT-SHOCK (Ref 4) that came a few years ago. Since it tried to tie the hands of interventionists, it was not very admired. It proved that, if an ACS patient is hemodynamic shock , don’t touch the non-culprit vessels. (Only a few crazy cardiologists, could extract a vital , but non existent fact from this study. That is, if you want to destabilize a hemodynamically stable ACS/STEMI, try multivessel PCI)
Pros and cons of multivesel PCI in STEMI
Pros are plenty, as we can churn out an RCT as we wish, while the cons are reserved for pessimists, but they are not often imaginary.
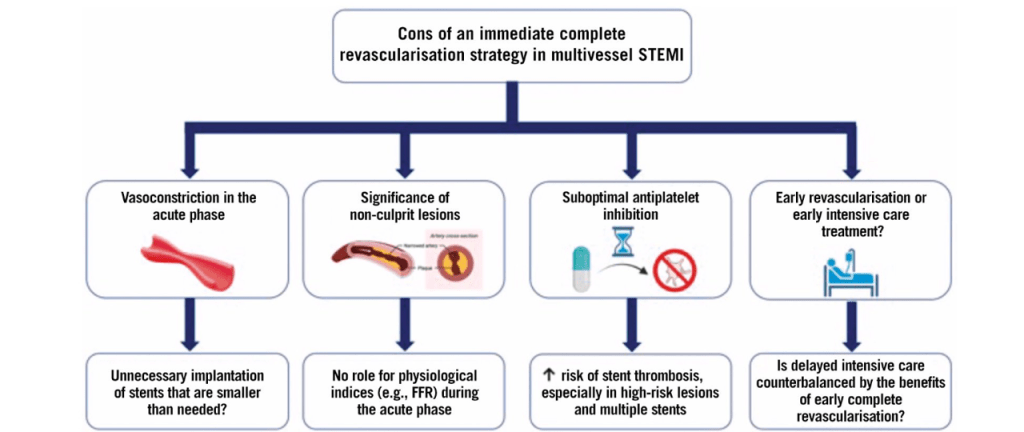
Immediate complete revascularisation after STEMI in patients with multivessel disease carries several important risks. Vasoconstriction during the acute phase may lead to unnecessary implantation of stents that are smaller than needed, potentially compromising long-term vessel patency. The assessment of non-culprit lesions is challenging in the acute setting; there is a distinct vasospastic component amplifying the lesion severity. Further there is no role for physiological indices like FFR to guide treatment, raising the possibility of unnecessary or inappropriate interventions.
Other significant concerns include suboptimal antiplatelet inhibition, which elevates the risk of stent thrombosis, especially in cases with high-risk lesions and multiple stents.
Finally, the decision to pursue early complete revascularization versus prioritizing intensive CCU care can be complex. A cath lab-centric thought process continuously interferes and clouds our intellect and common sense succumbs, i.e., an injured myocardium needs some rest after all, as do a tired cardiologist.
Final message
Should I fix that 80% LCX or 70% PDA in an anterior STEMI?
You are the boss in your lab, what you think must be right, because it is your thought. Also, you are licensed to do whatever you want to do in your patient. But, remember this: These lesions are not real culprits as of now, unless, The RCTs you love instigate them.
Cardiac failure mall of fame : Mounjaro wants to become another pillar !
Posted in Uncategorized on November 3, 2025|
The architecture of HF therapy recently went on a pillar building mode .Some are strong and evidence based , still, few of the pillars are still shaky. We know the terrain for pillar building in HFpEF is much more difficult . Now, Tirzepatide seems to be a God-made molecule. It is found to be useful in HFpEF. This study (Krüger N, et al Semaglutide and Tirzepatide in Patients With Heart Failure With Preserved Ejection Fraction. JAMA. 2025 ) is from Boston, Massachusetts, adding some credibility. Read yourself and to see whether it is really sturdy or shaky pillar.
The Gut-Heart connection
There is not much connection really. We want to connect it through Semaglutide and Tirzepatide through its antidiabetic and anti-obesity properties .How does this gut hormonal agents work in HF ? These drugs are analogues of glucagon-like peptide or gastric inhibitory polypeptide. These drugs can be called intestinal sedatives, slow down gastric emptying, reduce appetite, and hence weight loss and also diabetic control. They are secreted from K and L cells of the intestine.
The K cell the L cell (Kuhre RE, 2021 )
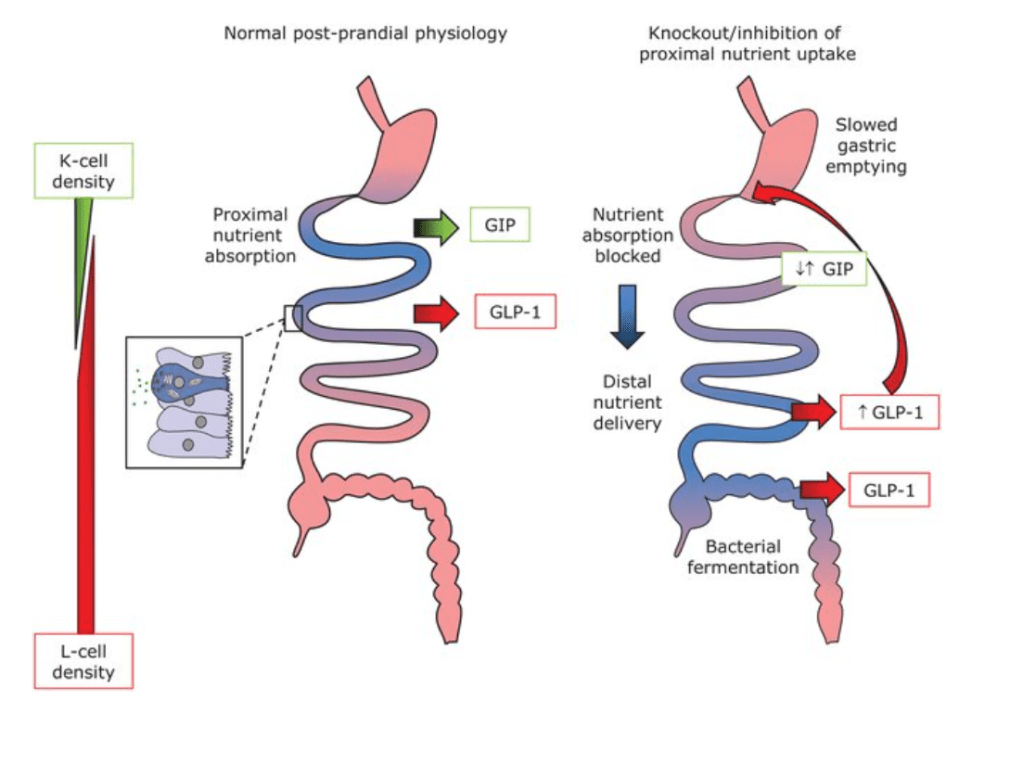
Glucose dependent insulinotropic polypeptide (GIP) is secreted from K cells, which are predominantly found in the duodenum, whereas glucagon-like peptide-1 (GLP-1) is secreted from L cells, which increase in numbers in the distal intestine. Both cell types are so-called open enteroendocrine cells with direct contact to the intestinal lumen, allowing sampling of the chyme and regulate food movement and modulate insulin secretion.
Final message
Weight reduction and diabetes control are indeed vital cogs in the management of both HFrEF as well as HFpEF (more so in the latter). There are number of simple, cheap and less-glamorous ways available to reduce weight.
At any point of imagination, Tirzepatide (Mounjaro) can not claim to be an anti-cardiac failure medication. Even SGLT-2 is just a glorified glycosuric drug, stealing the credit from diuretics .
It is important to realsie, as per our past track record, the side effects of all these weight losing drugs, would knock our doors, only after a year or two.
Reference