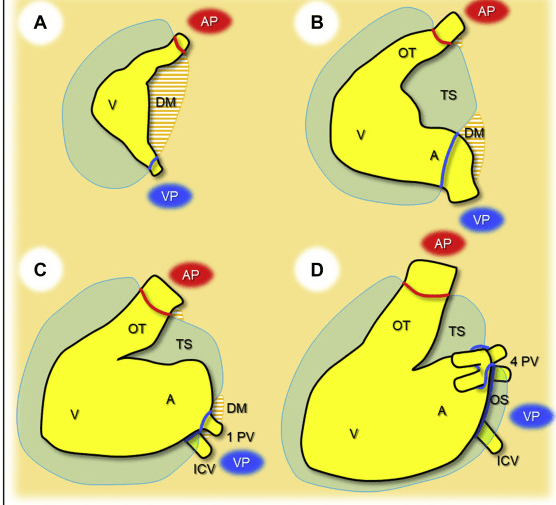
If you understand the pericardial anatomy fully, you can call yourself real master of clinical anatomy. (Ref 3,4) We know, it is a complex protective cover over the heart , that has three layers with a unique relation with one another. The outer one is tough conical bag .It has an embryologically distinct origin .It develops from septum transversum and sits over the diaphragm tightly, to which it shares the same embryological origin. While the inner serosal layer (rather cavity) splits into two layers and encloses the heart .Though this serosal layers develop from a different mesenchymal tissue , it is biological wonder both fuse in perfect harmony. , The developing heart bends, folds and loops within the serosal cavity.
The inner one embraces the heart fully forming epicardium (otherwise called visceral pericardium) and reflects back after covering great vessels .While reflecting back it is firmly attached to inner surface of fibrous pericardium forming the pericardial cavity . Never confuse parietal layer of serous pericardium with the thick outer fibrous pericardium, though both are gelled together. Since heart is not a strict globular organ, the hug of visceral pericardium over the heart is not uniform and complete , especially over the great vessels enter or leave the heart (Hilum of the heart). Hence it folds , and forms two sinuses and recesses.
What happens with pericardial Inflammation ?
Inflammatory pericarditis can occur in differential fashion. For example, the most common chronic pericarditis tuberculosis affects the fibrinous layer. Post MI pericarditis involves the epicardium. It is vital to understand epicardium is thin and transparent sheet of tissue , one may not split it from the heart. It is also important to know coronary arteries run under this thin visceral pericardium( ie sub epicardial) So anatomically , In constrictive pericarditis , the immediate target would appear to be the coronary artery , than the myocardium . But, what really happens ? Let us Introspect on this.
In CP which layer exerts the force of constriction ?
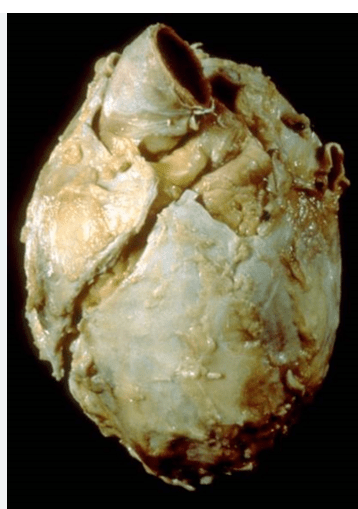
Macroscopically ,It would be a dramatic sight to see the heart caged within hard shell of pericardial mass. To be frank, we can never make a distinction between the three layers once its thickened. Which layer is the triggering force, that promotes adhesion and compression is also not clear. We presume, the thick fibrous layer is villain de chief. (This we learnt , by observing rheumatic heart disease pathology ,wherein pericarditis , never evolve into constriction as it doesn’t affect the thick fibrous layer) .The inflamed exudative pericardial fluid doubling up as a glue to stick all three layers is a true possibility.
Whatever happens, once the inflammation become chronic, it goes on steadily and begin to compress (rather restrict in diastole). At this stage, anti- inflammatory drugs like NSAIDS, colchicine or specific anti-tuberculous drugs along with a bit of steroids can arrest or slow down the pathological process and prevent this deadly disease. The phenomenon of transient constriction with normal thickness pericardium is also reported.
The normal and the pathologically thickened constrictive pericardium
The quantum of constrictive force widely varies in different areas of the heart. Obviously, the thickened pericardium hurts the heart in diastole . Right side of the heart is more vulnerable because of its thin wall and the low pressure beneath . However the constriction process continues over, anterior, lateral , posterior and even the AV groves The sinus the recesses can also become obliterated .
Does the coronary artery gets compressed ?
When the whole heart become as hard as a cricket ball , what do you expect the fate of coronary artery would be ? Fortunately, it escapes in many . But, the threat of compression or calcific (ice-berg) injury is always there. There has been many reports of patients with angina in CP (Ref 1). Here is case report from India , where a calcific pericardium exerts a vice like tightening over LCX. (Ref 2)

This is not surprising, when we know, at late stages the pericardium can even infiltrate the myocardium.
How do the coronary artery often escapes in CP ?
One important reason is , unlike myocardial bridge here the artery gets compressed in diastole , with a passive distending pressure from LV cavity rather than active constrictive force.(See the above video) The diastolic coronary arterial pressure rarely goes below intrapericardial space pressure , which in fact is obliterated. Still, the point to be noted is, mass effect can still result in non hemodynamic compression.
Final message
Fortunately, coronary arteries often escape from serious pressure effects of constriction but the threat is real especially in late stages .It can happen either by the calcific spurs in the pericardium or diffuse pressure effect or tight ring like localized constriction. While de-nova coronary Involvement is far less common, the operating surgeon needs to take extreme care to avoid it during surgery . Surgical pericardiectomy is either partial or total caries considerable mortality even today. Total pericardiectomy is myth at best. Few pieces of adherent pericardium are left over especially in the posterior aspect.
There is a landmark study from Mayo clinic, with data from over 1000 pericardiectmy surgeries ,over eight decades . Every cardiologist and cardiac surgeon must read this to understand the nuances of pericardial surgery (Murashita Ann Thorac Surg. 2017) Now Robots are being tried to assist in this delicate surgery (CTS-NET 2023 Total Robotic Pericardiectomy for Constrictive Pericarditis)
Reference
Two Excellent reference for comprehensive knowledge in pericardial anatomy