Statins belong to a group of drugs, stolen and reengineered from the blueprint of natural Chinese red yeast rice (Monocoline K) in the late 1980s. The rest is the remarkable history in the pharma industry.
Statins directly interrupt the cholesterol synthesis by blocking HMG-CoA within the hepatocytes. It significantly lowers the LDL, fights human vascular atherosclerosis. It makes the plaque either regress, prevent progress, make it harder and in the process make them less vulnerable . There are innumerable studies that document the evidence. Statin has become a must-prescribe drug in any one with clinically established CAD or even in concealed CAD. Guidelines are available to prescribe statins various intensity, depending on the risk profile.
Which statin ?
There has been a long list of statins. Many of them have retired from the ring .Currently, the fight is between Atorvastatin, a Rosuvastatin. Like Pepsi vs. Coke.
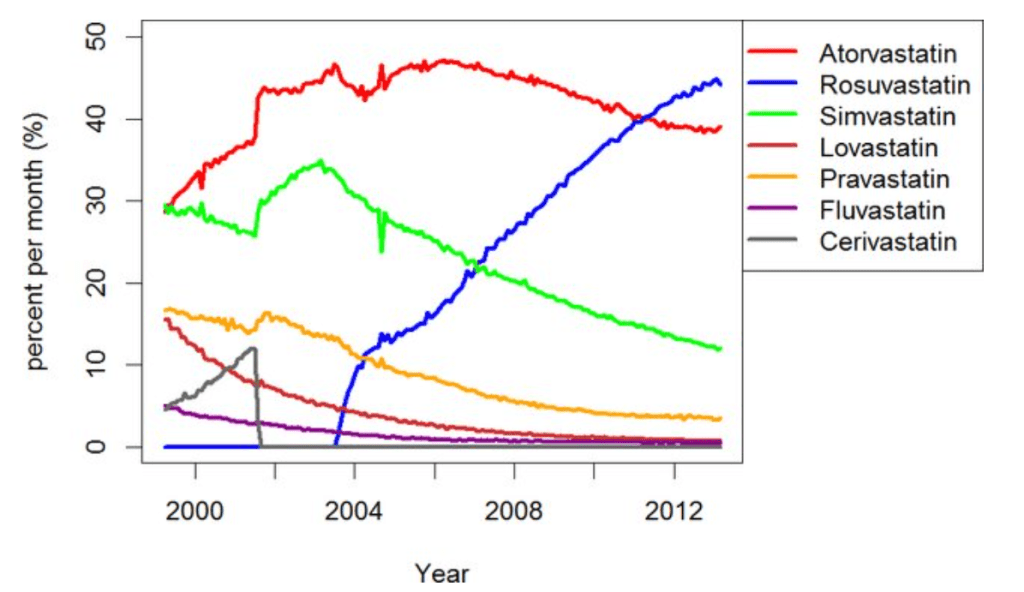
Note the graphic ,A meteoric rise of one drug since 2005 . (Can you guess the reason ?)
ATRORVA or ROSUVA Which one should I choose ?
There is very little “one to one” comparison study between Rosuvastatin and Atorvastatin .The gap in the pros and cons are narrow. Following points are observed, without much dispute.
1.Rosuvaststin is more powerful.
2.Plaque stabilisation effect is not different((Satrun, study NEJM 2011 based on IVUS)
3.New onset diabetic risk is more likely with Rosuvastatin
4.Worsening of cataract is also more with Rosuvastatin
5.Atrovastatin has some additional benefits in lowering triglycerides. (Bakker-Arkema RG, JAMA. 1996)
No one is dare enough to give strong verdict . Surprised to find one this month. BMJ has come out with a possible answer. It is called LODESTAR trial (Ref 1)
Mechanism of new onset diabetes with statins (REF 3)
It can be 7% with Rosuvastatin (less with Atorvastatin). We think, statins act primarily within the hepatocytes where cholesterol synthesis takes place, but they also have an eye on the pancreatic β-cells as well. It down-regulates GLUT-4 in adipocytes, and results in compromised insulin signalling. Furthermore, statins’ impact on epigenetics may also contribute to statin-induced T2DM via differential expression of microRNAs.
Mechanism of cataract with statins (Ref 2)
The cells lining that line the lens are dynamic and require cholesterol on a day-to-day basis. Statins inhibit proper epithelial cell development within the crystalline lens, where cholesterol biosynthesis is critical to maintain transparency and structure of the lens.
Final message
So, is it Atorvastatin or Rosuvastatin? It is left to you.
Mind you, “no statin at all” is the best option if circumstances and risk profile allows. Statins are never considered life-saving staple drugs in our fight with CAD and atherosclerosis. We, along with our scientists might may make you feel like that. Lipids can be controlled within desirable means exclusively with diet and exercise in most of the population* .
(*Forget about statins in the last 5000 years of known human existence, so many great people have lived a long and successful life in this world, without even knowing there is an organ called the heart that is responsible for the circulatory system)
Reference