For right or wrong reasons, the world of electrophysiology has pushed us into a belief system that, if it is AF, the culprit must be pulmonary veins. In fact, non-pulmonary vein origins can be a staggering 70% in some series. (See below) It can be in the free walls of the left atrium, LA appendage, IAS, IV, SVC junctions, coronary sinus, ligament of Marshall, crista terminalis, etc. (Ref 2)
For example , where will be the initial focal trigger for AF in a pateint with COPD ?
Can you ever think of ablating PVs in a patient with AF and COPD, where the right atrium is under stress and strain? It doesn’t require any extraordinary intelligence to conclude any chronic focal atrial tachycardia can get degenerated to AF in the long run. In that case, the famous atrial tachycardia localizing map from Peter Kistler et al from Australia JACC 2006 holds good for location AF focus too.
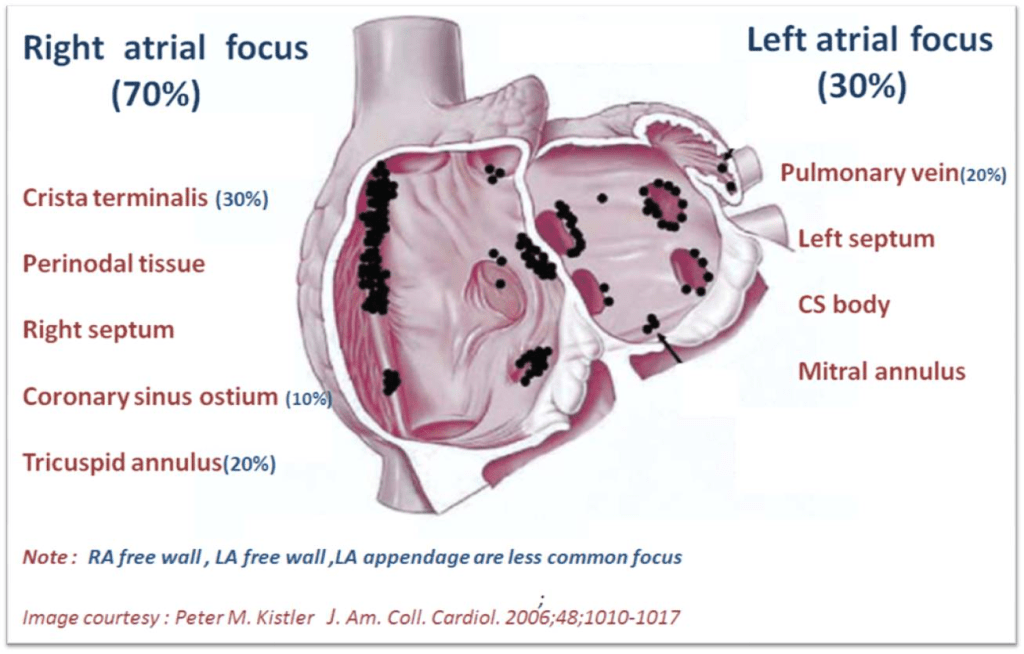
If we look at the above map,RA prevails over LA convincigly in termes of focal atrial tachycardia. Only 20% of focal AT arise from pulmonary veins. I guess, the same should be true for AF.
Focus-less Atrial fibrillation
Right from the days of James Mckenzie, when AF was refered to as delirium cordis or ataxia of pulse, AF was always considered as a chaotic, focus-less arrhythmia. It is still true in many cases. The recent pulmonary vein triggers are just a small revelation and need not be a revolutionary paradigm shift , as we are taught. There are innumerable patients who develop de-novo AF without any focus. Hypoxic or acidotic milleu of a single atrial myocyte can iniitiate an AF, alosan episode of atrial ischemia, diffuse inflammation as in atrial epi-myocardiits can trigger AF from any spot on the atrium.
Reference