The therapeutics of coronary stenosis has become a technogical wonder, interwoven with statistical wordplay in the last few decades. PCI is sitting pretty at its peak glory.The term OMT or GDMT is a popular terminology, but realistically exist only in guidelines.
It is a strange academic habit among cardiologists, that they have subdivided medical management into optimal and suboptimal. Meanwhile, we haven’t seen any papers from cardiology forums that classify PCI according to its quality. How many of use a term like optimal PCI or guideline-directed PCI (O-PCI, GDPCI). Every PCI, by default, is perceived as good by our flawed coronary intellect.
A single patient experience
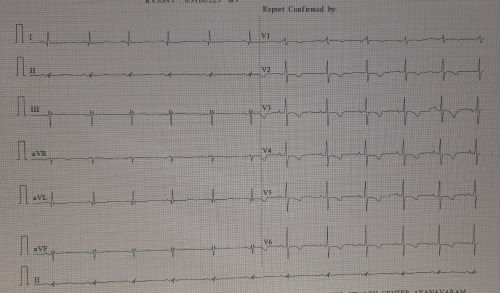
Let me share a patient consult from a remote town of north India. He is a STEMI patient (1 year old) with mild LV dysfunction and thinning of IVS and anterior wall. His CAG showed a significant looking, yet non-flow limiting LAD lesion without any troubling symptoms. I came to know he had consulted two institutions and was apparently not happy with their approach (In his own words, “They seem to be primarily interested in caging my LAD than listening to me”).
Somebody has suggested my name. He called me over the phone for a consult. I asked him remain there to follow his doctor’s advice. But, he flew some 2000 km to meet me. He was so knowledgeable and was aware of everything I wanted to tell. Like, viability, scars, futility, and benefits of revascularization, imaging-assisted PCI, impact of PCI on exercise capacity, importance of risk factor management, etc.
I told him, “In my opinion, you have technically a single vessel disease that can be managed well with drugs. But if PCI is to be done, it should be done in a proficient manner, as the lesion looked hard and was close to the LAD ostium, trespassing LCX as well.” I stressed the importance of a professionally done procedure with enough expertise and follow-up maintenance care.
He was not entirely satisfied with my response. He wanted a clear yes or no! . I told him, “If you have full trust, continue with the drugs at full intensity and do a stress test after 3 months. otherwise, if you keep getting even the slightest doubt and anxiety over the hidden blocks, go for a stent immediately at a good Institution. (My conscience said the latter half of my advice was unwarranted, but I had to; after all, me too need a protective mechanism)
He left my clinic profusley thanking me. I am not sure , how my consult was useful for him and what he is going to decide.
Academic lessons from this patient.
1.Patient fear factor over coronary blocks may be the ultimate game changer. Cardiologists should try to mitigate this fear and at the least should not be an amplifier to this emotion.
2.Leaving tricky profesionaly complex decisions to the patient, is an easy escape route for us, however it comes very close to professional incompetence. (Of course, we do this on a routine basis, approved by the modern medical guidelines, ethics, and legal system, in the name of patient empowerment)
3.Finally, we can grow a potential research hypothesis. A sub-optimal PCI is non-superior to OMT.It is curious there is no study available to compare sub-optimal PCI to OMT. We must also realize there is nothing called standalone PCI. Without concomitant OMT, PCI is a dud. Every young cardiology fellow need to etch this fact in their cortical cardiac memory. OMT often turns out to be the savior of stents, but the latter ruthlessly steals the credit.
Postamble
I could find one study analyzing suboptimal stenting (Ref 1), but it didn’t compare it with OMT. Suddenly, as I finish writing this, a big fact struck me hard, i.e., even a well-done PCI in sophisticated core labs with meticulous care struggled to beat OMT in a barrage of landmark trials (like COURAGE, ISCHEMIA, ORBITA). What is the big deal to analyze suboptimal PCI vs OMT?
Prati F, Romagnoli E, Gatto L, La Manna A, . Clinical Impact of Suboptimal Stenting and Residual Intrastent Plaque/Thrombus Protrusion in Patients With Acute Coronary Syndrome: The CLI-OPCI ACS Substudy Circ Cardiovasc Interv. 2016 Dec;9(12):e003726. .
Read Full Post »