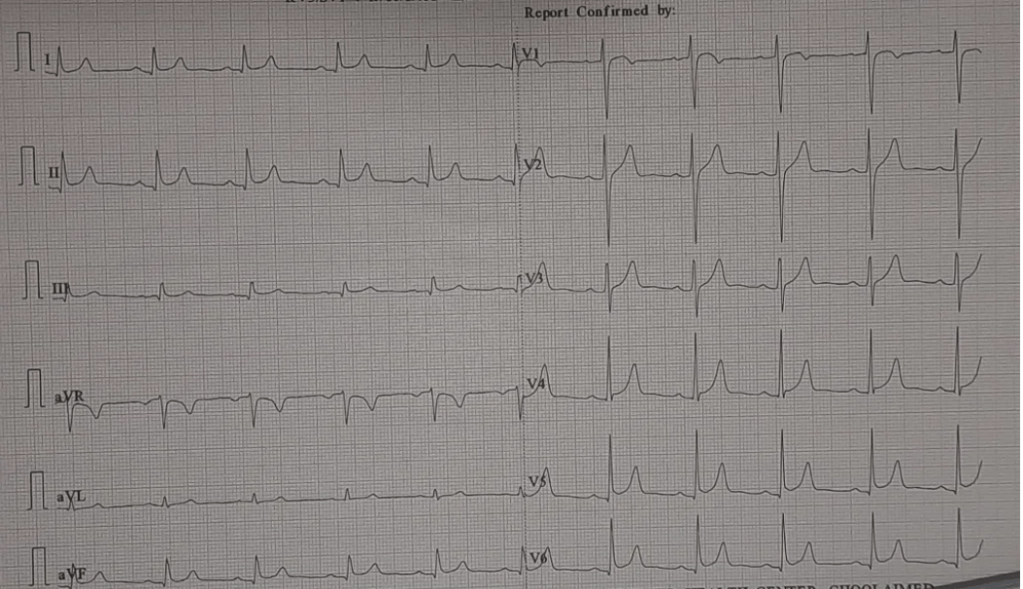
Right now, I am sitting at a yet another national conference on Interventional Cardiology. Two very popular cardiologists, from elite institutes of India are debating on a 60-feet long digital dais, with a flashy background comparable to the Macau skyline. Watching it, are about 600 prosperous delegates , brought from various parts of India. The debate is about, whether to use a single stent or upfront two stent strategy for left main bifurcation disease. The arguments were all too familiar, I just couldn’t concentrate.
I am sure every one will agree ,this topic is being debated for nearly two decades. The answer, we got is crystal clear. 90 % of BFL need just provisional single stent. Rest may require two stents upfront. The quality of the procedure matters more than the technique. Not even Imaging matters much. Of course, we are free to choose DK or various other forms of crush as we like. That’s it. May be, It’s time to we close the shutters on the exclusive and glamorous bifurcation clubs and move on. (until a real Innovation in dedicated bi-furcation stent happens)
The following add on was not part of the debate
*Before any BFL PCI, spend a few silent moments, while the patient is being laid on the cath table . Whether the patient is truly symptomatic, whether he could be a candidate for simple medical management or his lesions are complex enough to deserve a CABG.
Final message
Beginning to wonder, is there a fundamental problem with the current mode of knowledge flow and consumption in the field of cardiology. Why do we keep plagiarizing the same old content in the conferences year after year in spite of being fully aware of the futility? This raises a fundamental issue. As we learn more & more, is there a risk of our wisdom curve getting blunted?