A brief learning session with cardiology fellow about a possible new concept in Left heart failure.
What is the commmest cause for acute pulmonary edema?
“Left sided heart failure”
“Can you be more specific , Left sided means ?
“I meant LV failure , typically DCM of any cause or Severe un-controlled HT”
“Ok .good. Does Left Heart failure include mitral valve dysfunction also ?
“Yes sir, very much. Classical mitral stenosis and Isolated MR can cause pulmonary edema. In fact, acute AR Iis also part of left heart disease”
So far, so good, now coming to the complex part of left heart
Can LA fail in isolation independent of LV , ie I mean with normal Left ventricle ?
I am not sure. Can we call new onset atrial fibrillation as a primary atrial failure that can result in pulmonary edema?
Excellent. You are absolutely right. But I am talking about mechanical atrial failure, not electrical. Are you aware that most of the time AF is a well tolerated arrhythmia , it can even be silent in many cases. This is because the pumping function of the atria contributes only 20-25% to LV filling. This can easily be compensated by augmented LV suction force , provided the baseline LV function is normal.
Have you heard about ACM. Atial cardiomyopathy?
“No sir”,
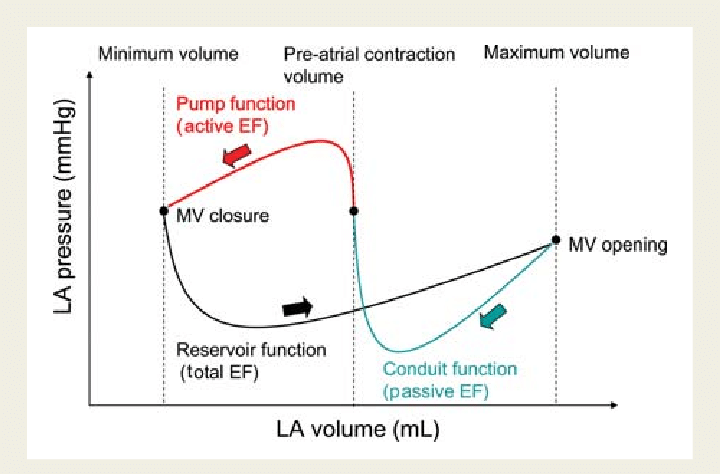
“You will hear more about it soon” (Ref 1) Scientists, especially Echo guys are closing in on this concept. We know, the atria has three functional components, namely conduit, reservoir, and pumping. Curiously, we have realized that the pumping function of LA may not be that critical from indirect observations from some land mark studies . (Rate control vs rhythm control studies in AF are a powerful proof on the atrial pumping function .(AFFIRM/RACE etc ) I don’t know, whether I am right in saying the above statement.
It is tempting to conclude , only if all the three functional components of atria gets affected , then only primary atrial dysfunction can be diagnosed. The concept is more complex than we realise. In diastole , pulmonary vein, LA , LV all work as single functional unit. Only in systole, we see them as different things.
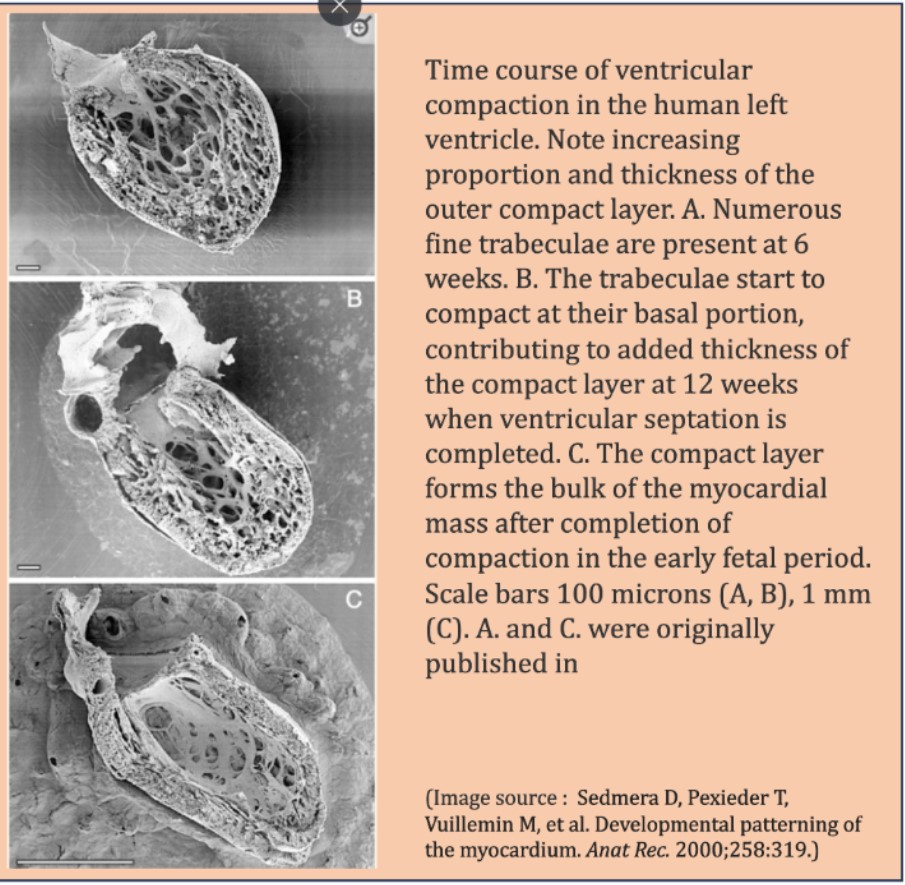
Atrial DCM
Like LV systolic function, which is coupled with RV in parallel , LA function is closely knitted to LV in series during diastole. The key to suspect or diagnose this entity is to demonstrate dissociation of LVEDP with LA mean pressure & PCWP. This is not an easy job in bedside. Isolated Increase in LA volume without any reason , is one clue. LA ejection fraction is possible marker. (Kanagala P, . Int J Cardiovasc Imaging. 2020)
Final message
We are in the early days of understanding primary atrial mechanical failure, Atrial cardiomyopathy (ACM) or atrial DCM is being proposed as separate entity. It is very likely, some subsets of HFpEF might turn out to be primary atrial disease, depending on the level of investigation we do.
Reference