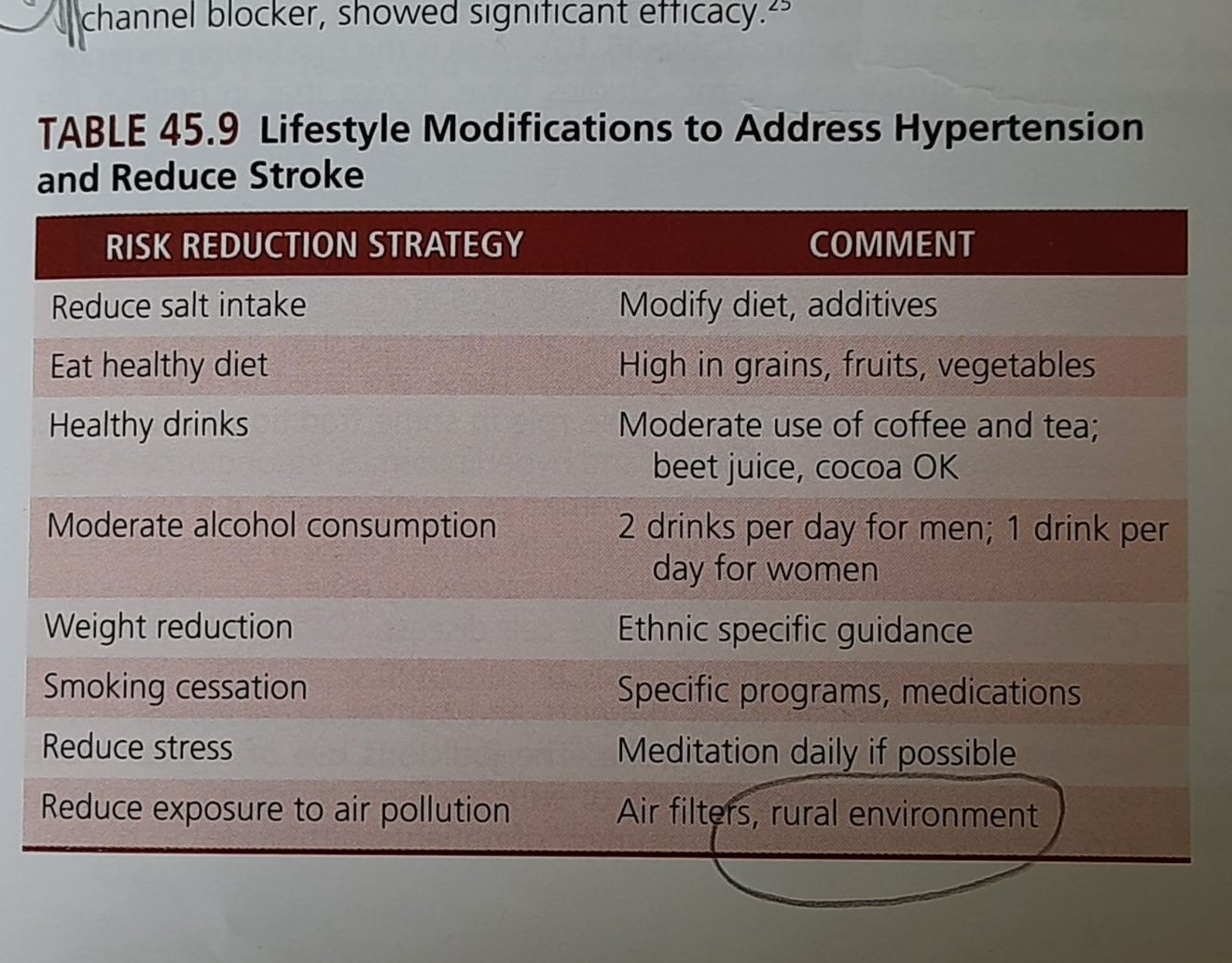
(Why should the number 65 bother us in TCFA-detected by OCT? Does this number really deserve that respect? Trying to find some truths from 8 questions with & without evidence.)
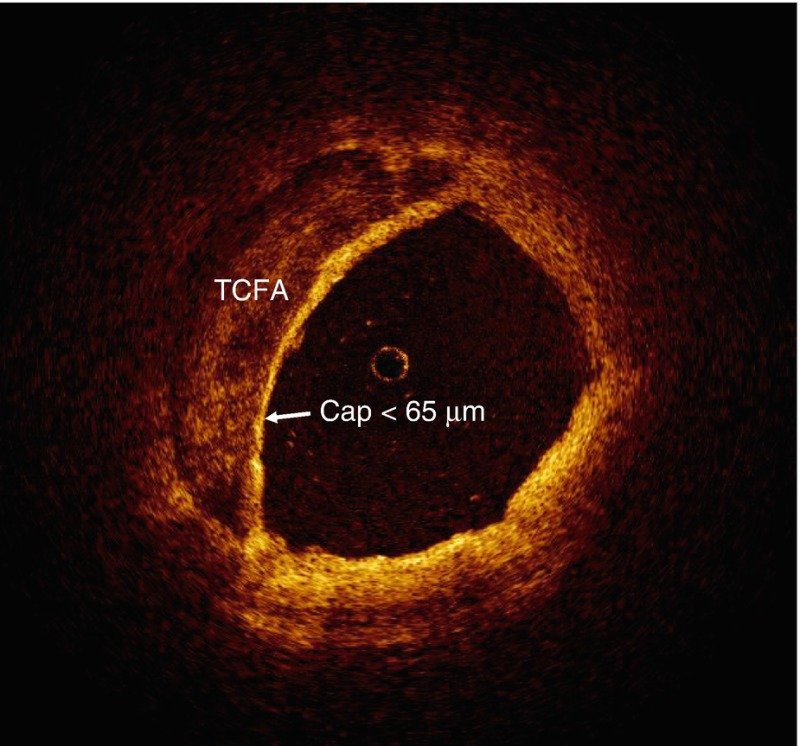
1. Does TCFA really make a plaque vulnerable?
A.Yes
B. No
C. Maybe
Answer: Yes & Maybe. But there seem to be more important factors other than TCFA for a plaque to become vulnerable making TCFA not really a big deal.
2. TCFP is more common in which lesions?
A.Flow limiting lesion
B.Nonflow limiting lesion
C.No relationship between TCFA and flow
Answer: No relation, rather a random relationship.
3. What is the natural history of TCFA?
A.Get ruptured
B.Static
C.Get thickened
D.Further thinning
Answer: If someone can answer this query accurately, he can be rewarded Nobel Prize, in Lipidology
There are some studies available though.
Ref : This 2023 paper adds some anxious content to those who ignore TCFA. Long-term outcomes of patients with normal fractional flow reserve and thin-cap fibroatheroma EuroIntervention 2023;18:e1099-e1107. DOI: 10.4244/EIJ-D-22-00306
4. What to do with FFR-negative(FFR>.9), TCFA-positive lesions (tcfa<50mic)? Does stenting TCFA make it less vulnerable?
No. Stents and scaffolds were never invented to make a plaque less vulnerable.
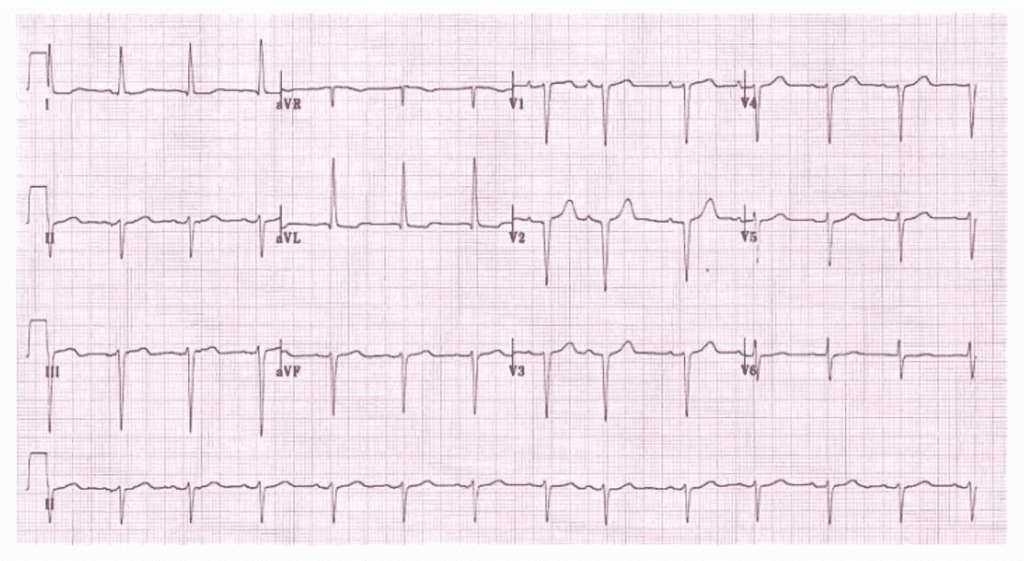
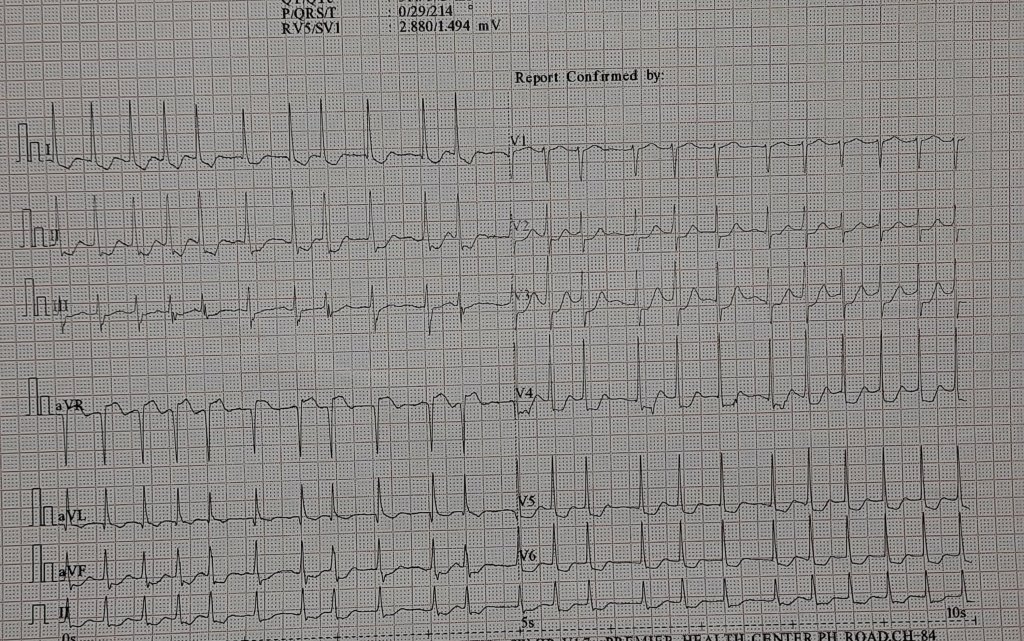
5. How is TCFA different in stable CAD from ACS situation?
They are very different. In the ACS situation, TCFA (Whether the cap is intact or not ) needs immediate attention. Does it mean immediate stenting? No, it is not. (But unfortunately, it is what happens in the reality.) Thrombus and its lytic products add a new dimension of risk for recurrent ACS. High-dose statins are critical here. Stenting is so tempting, and logic and science are in direct conflict here.
6. Do statins increase the thickness of TCFA?
A.No
B.Yes
C.Possibly yes.
Answer: Statin does have some action on the cap. there is no such thing as if the cap increase from 65 to 100 micron the plaque is safe. More than thickness, it stabilizes and hardens the contents that are being capped. European Heart Journal – Cardiovascular Imaging (2017) 0, 1–8 doi:10.1093/ehjci/jex102
7. Which is possibly, the thickest cap over an atheroma?
Intimal calcification on the luminal side is the thickest cap (like a helmeted plaque) that protects from any traumatic injury from blood components. (Sub Intimal calcific nodules may behave differently though)
8. If calcium is the safest cap in chronic CAD,, why do cardiologists, attack it with all sorts of weapons?
This is where “excessive knowledge along with academic ego‘ in incognito mode plays spoilsport with our hidden wisdom.
Calcium is an uninvited guest that directly challenges our might and talent, and interferes with placing a stent. No surprise, we take up this fight personally, and destroy, shock, drill, or displace it at any cost. Of course, tackling calcium* is required in very selected patients; it should never be done just because it interferes with the deployment of a stent. (We need to periodically remind ourselves, that PCI is not synonymous with stent implantation; stentless PCI is also possible.)
*Calcium and coronary artery is not a simple topic to understand. How can one agree with the above content, when there are innumerable studies that say a high CT calcium score is directly related to plaque burden. Mind you CT calcium score has little correlation with intimal plaque rupture.
TCFA: Should we worry?
TCFA is a concept born out of cutting-edge coronary Imaging technology OCT. After a decade of experience, we realize we can’t hunt & count these caps among the vast plaque burden. The 65-micron cap is just an anxiety-provoking number. Forget the cap. They are often Innocent.
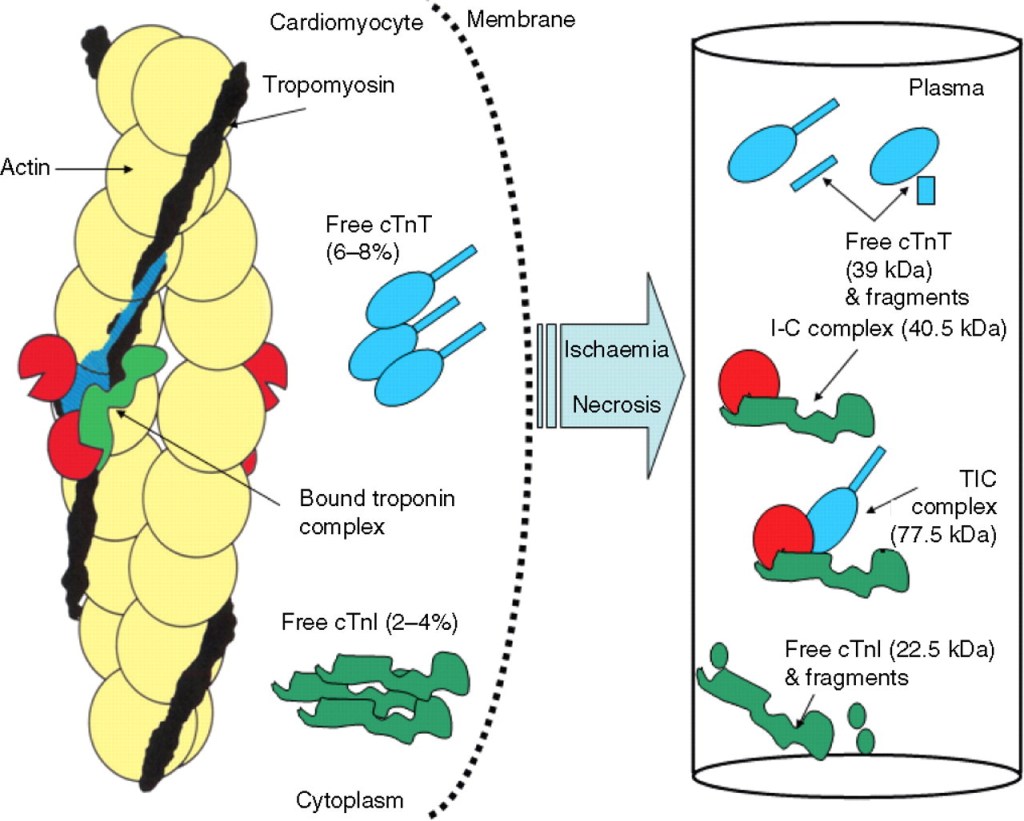
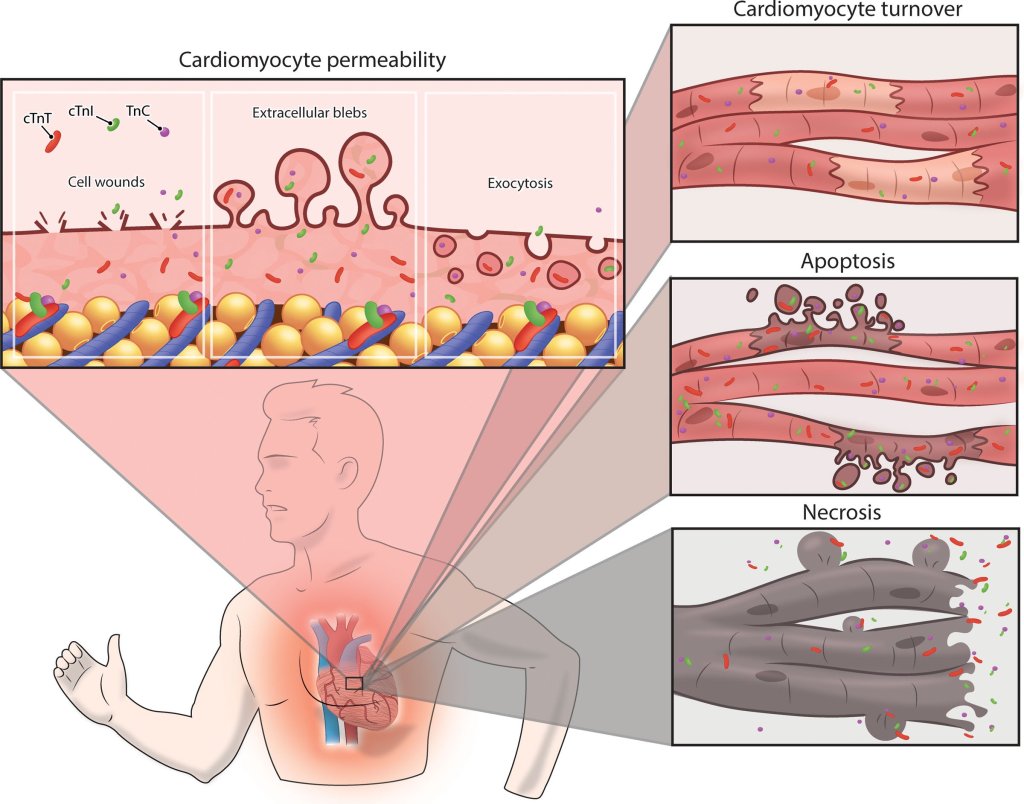
Looking beyond TCA
What is beneath the cap and the biomechanical forces in the pool of tissue underneath, ultimately matter. The fluidity of the necrotic core and the ferocity of the angry macrophages, MMPs, as well as the triggers from within the lumen like the shear stress of blood plays a major role. We also know that diabetic glycation injury widens inter endothelial gap. We have sufficient reasons to assume, that the sharp edges of LDL molecules, hit the endothelium at a high mean BP along with neural triggers from the peri adventitial sympathetic network that injects the final catecholamine blow to the endothelium.
Final message
No technology can answer the above queries or predict the events. So be at peace with all basic precautions and risk factor regulation.
Reference
1.EuroIntervention 2023;18:e1099-e1107. DOI: 10.4244/EIJ-D-22-00306
2.European Heart Journal – Cardiovascular Imaging (2017) 0, 1–8 doi:10.1093/ehjci/jex102