
.
Post-amble
Are you a professional physician doctor ?
Honestly I am struggling to become one , it is still a long way to go.

.
Post-amble
Are you a professional physician doctor ?
Honestly I am struggling to become one , it is still a long way to go.
Posted in Uncategorized | Tagged bmj, ethics in cardiology, ethics in medicine, Hippocratic oath, jama network, lancet, medical ethics quotes, nejm, who is a professional cardiologist |
Open artery hypothesis
The open artery hypothesis was first postulated by Eugene Braunwald in 1993 (Ref 1). He suggested that restoring blood flow in an occluded coronary artery, has time independent benefits. beyond the acute phase of myocardial infarction. The proposal was, it could improve left ventricular function, reduce remodeling, and potentially decrease mortality by mechanisms beyond myocardial salvage, such as reduced ventricular arrhythmias and improved healing and also potential channels of future collaterals.It was a great concept and sounded very logical and got world wide attention.
Is it really valid now as a therapeutic concept in CCS ? If so, why we struggle to show benefits in asymptomatic CTOs ?
The fact that, opening a CTO is not bringing the expected benefits is one of the most intellectual questions in coronary physiology. Most of us are not keen to go deep into this question.
Now get ready for some nasty truths. There are plausible mechanisms by which opening a CTO might increase the risk of recurrent events compared to a stable, closed artery.
1.Procedural Risks:
CTO-PCI is technically complex, with risks including periprocedural myocardial infarction ,coronary perforation, stent thrombosis, restenosis, and contrast-induced nephropathy. In this context , it is worth noting the DECISION-CTO trial reported a 2-3% rate of major procedural complications, which could of offset benefits of PCI in asymptomatic patients.
2.Restored Flow and Plaque Instability:
Opening a CTO restores blood flow to a previously ischemic territory, but the downstream vessel may have unstable or vulnerable plaques that were previously “protected” by the occlusion. Sudden reperfusion could trigger microembolization, increasing the risk of acute coronary syndromes (ACS).
3 .Stent-Related Issues:
CTO-PCI often requires not only long procedure times, it often requires long stents , or multiple stents, increasing the risk of stent thrombosis compared to a naturally occluded artery that has adapted with collaterals. Dual antiplatelet therapy (DAPT) post-PCI introduces bleeding risks, which may outweigh benefits in asymptomatic patients.
4.Collateral Regression:
CTOs often develop robust collateral circulation, which may provide adequate perfusion to the myocardium. After successful PCI, collaterals may regress, leaving the myocardium dependent on the newly opened vessel. If restenosis or reocclusion occurs, this could lead to ischemia or infarction, potentially worse than the pre-PCI state fed by the caring collaterals.
5. Inflammatory Response:
PCI also induces an inflammatory response in the vessel wall, which may promote neointimal hyperplasia or accelerate atherosclerosis in the treated segment, increasing the risk of future events. All these, bring a curious and serious assumption close to reality. (That is, opening a CTO could, in some cases, disrupt a stable, quiescent milieu into, potentially un-predictable terrain and lead to more events than leaving the artery closed.)
The lack of clear benefit from CTO-PCI in asymptomatic patients, as seen in trials like the Occluded Artery Trial (OAT) and DECISION-CTO, may partly stem from these risks. Key reasons include:
While no study has explicitly tested whether closed arteries are better than open ones , several trials and analyses have explored whether CTO-PCI increases event rates compared to leaving the artery closed.
Occluded Artery Trial (OAT)
DECISION-CTO Trial
EXPLORE Trial
Thanks to the absolute democracy in science , I can propose a concept, however crazy it may appear. Yes, it is the Closed artery hypothesis . It can be defined as follows: In asymptomatic patients with chronic total occlusions and well-developed collaterals, leaving the occluded artery closed may result in fewer recurrent cardiovascular events than opening it via PCI, due to the stability of the collateralized system and the risks associated with intervention.
The closed artery hypothesis could turn out to be a compelling concept that merits further investigation
Reference
Postamble
What makes coronary blood flow dynamics so fascinating ?
A cardiologist’s primary job is to open the artery when it is closed in an emergency . This rule goes topsy-turvy when it happens in a chronic fashion**. Think about the two contrasting behavior of the same myocardium. In Stemi, it bounces back to life with emergent opening of the artery, while in the other, myocardium simply doesn’t bother about total shut down and possibly enjoys* the protection conferred by a closed artery.
*Objection my Lord. The word enjoys is brutal .Are you aware CTOs can be responsible for Stemi too ? ** But, Is it not Intriguing to note, OAT study included primarily ACS population and it looks so true , even acutely occluded coronary artery need some rest from reperfusion Injury.
Posted in Uncategorized | Tagged acc aha, closed artery hypothesis, collaterlas in cto, cto, cto guidelines, esc guidlones forpci, explore decision cto, jacto score, oat trail, open artery trial, opn artery hypothesis |
It is often said, If you are not able to answer a question, in a single line, or if the explanation is too long, then the answer is likely to be vague and difficult. So does this question.
It is a very practical probelm in day to day cardiology practice faced by every one of us. Still, it is often taken for granted during echo lessons in cardiology schools.
Here is a big table of differences listed. Read it if you have time.
There are only three words important. Find it out.
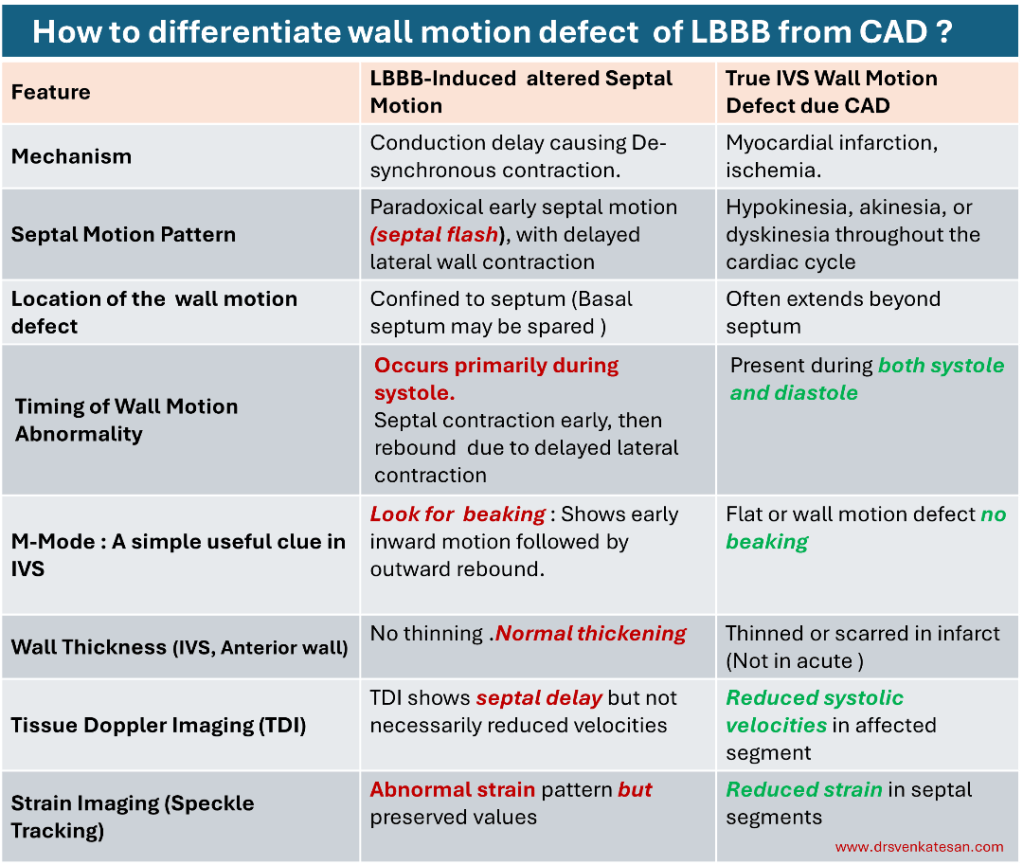
Final message
Look beyond septum, concentrate both systole and diastole. Normal systolic thickening and beaking in M-mode, clinch the diagnosis as LBBB
A query for advanced readers.
If LBBB and CAD /DCM co-exists, (a common scenario ) Which component of wall motion defect dominates ?
The answer to this question becomes important, as only the electrical component is correctable by CRT (or CSP now). No surprise, there is huge chunk of non responders, where myocardial component of de-synchrony prevails over the electrical LBBB,
Posted in Uncategorized | Tagged crt in lbbb, csp for lbbb, csp vs crt, dcm and lbbb, paradoxical wall motion defect in lbbb, septal beaking, septal flash, systolic wall thickening, wall motion defect in lbbb vs cad |
History beckons… once upon a time, assessing severity in valvular heart disease was gloriously simple. We used to just a pullback pressure gradient across the aortic valve . Now, history repeats itself, as the same philosophy returns to coronary arteries, offering a surprisingly elegant solution amid a chaos of physiological indices. That is PPG .
Pullback Pressure Gradient (PPG) is a physiological mapping method that evaluates the pressure gradient across a coronary artery using a gradual pullback of a pressure wire . It helps to:
Rather than a strict binary verdict (ischemic or not), PPG gives us a gradient map — revealing how pressure falls, where it falls, and whether intervention makes sense.
*I would love to call it as plain old PPG. POPP-G . (Sort of POBA equivalent in PCI)
PPG is a dynamic, localized, gradient-based insight into coronary disease. A focal ΔP over small length ΔL would be a perfect PCI candidate. A flat gradient over long ΔL , would suggest medical therapy .(May be CABG in few)
How do you FFR in bifurcation or trifurcation lesions . If you ask this question to any cardiologist, will try to get away from the scene. Such is the complexity involved. Here comes the savior. PPG helps you out in a smart fashion.
Image courtesy : Daniel Munhoz CARDIAC INTERVENTIONS TODAY MAY/JUNE 2021 VOL. 15, NO. 3
FFR was a great concept when it came in. FAME I study adored It. FAME II questioned PCI’s benefit despite FFR-positive lesions. Then came DEFINE-FLAIR and iFR-SWEDEHEART, questioning the need for hyperemia at all. Still, residual ischemia post-PCI in up to 20% of cases (DEFINE-PCI) even when FFR said “normal.” Confused? So are most cardiologists.
The list is long . FFR , iFR, FFR-CT, QFR, RFR, dPR, NHPR, µQFR (there are few more I might have left ) . None are perfect. Some contradict. Some cost too much. Many need drugs. All add layers of complexity to what should be a simple clinical question: Should I stent this lesion? Now, we have the simple plain PPG.
Let’s be honest. PPG is not flawless. After all, we take pressure drop as a surrogate marker for restricted flow . Every Indices does that. But unlike other indices It’s intuitive. It’s visual. It tells you where to treat. It gets the pressure data on the spot from ground zero . It can bring reliable info without the need for intracoronary medication , or costly software. Finally, it restores some simple sense in us ,without great knowledge in coronary hemodynamics.
Posted in Uncategorized | Tagged coronary flow reserve, ct ffr, fame 1 2 study define -flair study, ffr, hyperemic flow indices, ifr, Intermediate coronary lesion, non hyperemic indices, ppg, pull back pressure gradient, qfr, rfr, swede heart study |
Recently , a young celebrity lost his life during gym session suddenly . The media erupted as expected .Every TV channel became a temporary schools of advanced cardiology . It seemed anchors knew more cardiology than us.
Among the peers, so many hypothesis were going around. The loudest one was prolonged QT. We are discussing a relatively new, (rather les popular ) entity for the potential cause of SCD. What is it ? DID is the new buzzword in electrophysiology . Next to Long QT, Brugada, DID is looked upon as a new marker for SCD in young as well as elderly .
What is DID ?
Delayed Intrinsicoid deflection. (DID) Mind you, Intrinsicoid deflection ( ID ) is nearly 100 year old concept, being rediscovered. ID is the time it takes for the electrical impulse to travel from the endocardium to the epicardium directly beneath the recording electrode.
1.How to measure, what is the normal ?
Variable in each lead.
2. Which lead it is measure ? Is ID relevant in Limb leads ?
V5, V6. Normal less than 50 ms
3.When do you call Intrinsicoid deflection as prolonged ?
>50ms
4.What is the Ionic basis of ID ?
Sodium
5.Is there both congenital and acquired forms?
Yes
7.Is it different over RV vs LV ?
Yes
6.How does a DID trigger an arrhythmia ?
Not clear
Two more questions
7.Why it is called Intrinsicoid deflection rather than Intrinsic ?
Intrinsic was the original term coined by Sir Thomas Lewis in 1914, To get this “intrinsic” measurement, an electrode had to be placed in direct contact with the epicardium . Measuring it from surface ECG leds make it Intrinsicoid.
8. Is Intrinsicoid deflection and ventricular activation time (VAT) both are same ?
Yes. Both are used inter changeably , though one denotes time other the wave as such. While VAT is the same time , specifically look at time to R wave peak. However , ID can be applied to the leads where there is no R wave. Then it becomes time to peak of Q
9.Is it true, in every LBBB, ID is prolonged by default ? Then what is the risk of SCD in LBBB ?
For the first part of the question, the answer is Yes. The second part , we don’t know the true risk yet.
10. …………………………………………………………………..(Question left for the readers to ask)
Final message
As cardiologists, we have given disproportionate importance to the QT interval and gets the blame for many SCD. It is time, the 100 year old ECG parameter Intrinsicoid deflection (ID,) seems to be equally important. Much of the secret ionic codes, for many SCDs are believed to hide behind this eerie deflection.
Reference
Here is an important review
Posted in Uncategorized | Tagged brugada, delayed intrinsicoid deflection, did, id vs vat, LONG QT SYNDROME, ventricular activation time |
Once the Noble and pride profession, practicing medicine is becoming fearsome. India’s healthcare system is facing a silent emergency, not of disease, but of distrust. A worrying wave of rising intolerance among patients has led to an alarming surge in verbal abuse, threats, and physical assaults on doctors. Once revered as lifesavers, doctors now work under the looming shadow of mob rage, fueled by unrealistic expectations and social media-triggered misinformation. Emergency rooms have become battlegrounds. This is not just a law and order crisis—it is a near collapse of the doctor-patient relationship, once sacred, now strained to the breaking point. Urgent systemic, legal, and cultural interventions are no longer optional they are are matter of survival.
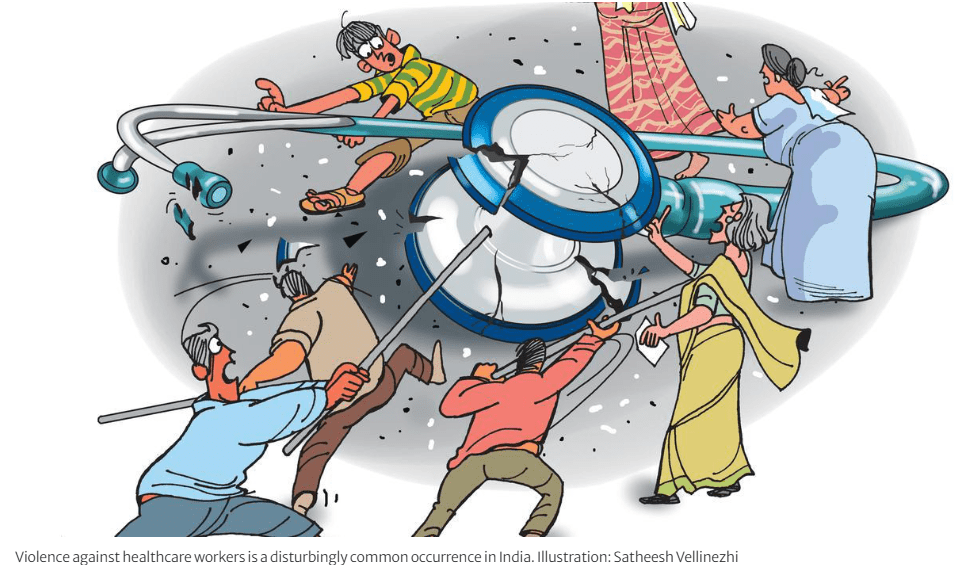
While the issue looks monstrous, if we dwell a little deeper, it is clear case of miscommunication, over-expectations, low tolerance, and sheer ignorance about human biology and illness . With the destructive mass of information explosion , every patient tries to think more than a doctor, about his or her illness.
This curious thought popped up during a debate with my colleagues . Why not propose a Hippocratic-like oath for every patient and their close family members as they enter any public or private hospital .Hippocrates would have never Imagined , there would be need for such an oath from patients.
Here is the Hippocratic Oath : Patient version 2025 : *Disclaimer : The content is never meant to underestimate the freedom and rights of the patients. While the patients are becoming hyper educated , with various resources , this oath is an attempt to enlighten them some simple but Invisible truths in our profession.
I am sure, this might look harsh, provocative, and even belittling of patient rights. But, to my conscience, it looks like, we the doctors have failed the whole patient population, by behaving, as if we are doing the job of a God. (at least in India) In the process, we have hidden many errors and systemic malfunction that are built into the system. We hesitate to tell the truth .For example . the true medical risk is dynamic and can vary moment to moment, even with an apparently simple procedure. (1% risk can become 100% risk in a flash ( A minor lapse of concentration* during a complex surgery or procedure can lead to… )
No surprise, patients expect 0% error and 100% success. Think for a minute and reflect. When did you last admit to your patient, “Yes, it was a mistake or error on my part?” That’s where the seeds of problems germinate. In spite of the dedication (& sacrifice) of our entire lifetime to our patients, we stand sorry. We must ensure and sensitize our patients, that complications and errors are irreversible attachments of disease and the treatment process. (As of now, so called informed consent document in India, doesn’t even receive the respect of torn rubbish in the dustbin.)
Reference
*Full time sports professionals like Messi or Ronaldo can miss a penalty kick in a most crazy fashion, Virat Kholi can see his middle stump flying on the first ball, but Doctors can never err* … they need to be perennially precise, 24/7 X 365 .How fair it is ? Wish, God shall answer this query for our beloved patients.
** But, the truth is , they err quite often is the untold story .The day our beloved patients realize this, medical profession will be released from the clutches of distrust from the patients.
Posted in Uncategorized |
Dr. Venkatesan Sangareddi MD, Former professor of cardiology, Madras medical college,Chennai .India
Medical science remains a cornerstone of human progress, and what we have achieved in the last 100 years is unprecedented. Every one of us is aware that the trust placed in medical research is sacred. Also, the medical profession is expected to remain noble as long as human beings exist. However, as in all walks of life, there must be trade-offs to any positives. Yes, this trust has increasingly become vulnerable, threatened by the pervasive and often subtle influence of conflicts of interest (COI). This is especially explicit in the current medical research landscape.
While the scientific community has made strides in acknowledging and requiring disclosure of COIs, particularly from authors , the measures are proving insufficient. There is a big irony sitting right across us. It is made to look, as if conflicts of Interest (COI) exist only with the authors.
The following article written by the author (Ref 1) calls for an awakening to every medical journal publishers, regardless of their prestige or impact factor, to recognize their vulnerability . We are expected to adopt a new paradigm of transparency in declaring COI, that extends to every participant in the publication process, including the scientific or ethical committies that approve the study ,the peer reviewers, the publishers and finally to the industries that fund the research.
Reference
1,Click here to download the full paper: A caution: It is a fairly lengthy article. (15 minutes read) Hope the suggestions made in the article are not labeled as unrealistic and possibly crazy as well.
Posted in Uncategorized | Tagged bmj, conflict of interest, jacc, jama network, lancet, medical ethics, nejm |
Measurement of pulmonary vascular resistance (PVR) is traditionally done by cardiac catheterization. It remains the (un)disputed gold standard, despite numerous assumptions, errors in measurement, and lack of reproducibility.
PVR by Echocardiography
Recently, echocardiographic calculation of PVR gained importance. Resistance is pressure divided by flow. Pressure is measured by Doppler, flow is measured by the cross-sectional area of RVOT times the TVI. We can arrive at PVR quickly. As simple as that.
Still, many institutions and purists ( Who have huge trust in cath derived, Oxygen diluted data) ) won’t accept this as standard . They fail to realise echo methodology carries less limitation, if not similar limitations as in traditional cath method. However, a significant advantage is, it is more real -time, can be repeated any number of times, and documents a baseline PVR, and at least is useful for follow-up.
There are two formulas used.
1.Abbas Formula
PVR = (TRV / RVOT VTI) × 10 + 0.16
2.Haddad formula :
PVR= (TRV²/VTI_RVOT)
*TRV = Tricuspid Regurgitation Velocity (m/s)
*RVOT VTI = Right Ventricular Outflow Tract Velocity Time Integral (cm)
Comparing Abbas vs Haddad
The Abbas formula is better validated and widely used in clinical practice, as it was specifically designed to correlate with catheter-based pulmonary vascular resistance measurements. It provides reasonably accurate estimates, especially for screening pulmonary hypertension, though it tends to under-estimate PVR at higher values (>8–10 Wood units).
In contrast, the Haddad formula ) is simpler but less rigorously validated and is more commonly applied in research settings focused on right ventricular-pulmonary artery coupling rather than direct PVR estimation.
Haddad’s method may be less reliable in patients with significant tricuspid or pulmonary valve abnormalities. Therefore, Abbas remains the preferred formula for routine clinical application. There is still hope to improve Haddad equation.
How to improve upon Haddad equation* ?
The Haddad equation for estimating PVR (TRV²/RVOT VTI) lacks calibration and overlooks key hemodynamic variables. It can be improved by introducing empirically derived correction factors to correlate with catheter-based values. Incorporating right atrial pressure (RAP), RV functional indices like TAPSE or RV strain, and adjusting for heart rate or rhythm variability can enhance accuracy. Averaging VTI across multiple cardiac cycles could also stabilize measurements. Additionally, machine learning on large datasets and AI-enhanced model could outperform the current linear Haddad formula for non-invasive PVR estimation.
* This is a fresh area of study , young fellows should come forward to do.
Final message
As discussed earlier, Abbas remains the preferred formula. But, the real issue is cardiologists refusing to accept any Echo-derived PVR and incorporate it, in the day to day practice. We have accepted EF % as the gold standard for LV function in spite of some serious lacunae. PVR carries the same story. Cath-derived data, in all likelihood, is enjoying pseudo-sanctity. It is time we should embrace one of these Echo formulas regularly and make life simple for both ourselves and the patients (who are often tiny babies or children). I think it can be done without compromise on scientific purity.
Reference
Posted in Uncategorized | Tagged abbas formula for pvr echo, abbas vs haddad, haddad formula for pvr pulmonary, normal pulmonary vascular resistance, pulmonary hypertension, pulmonary vascular ressitance, PVR by echo, wood units pvr |
None exposes the expertise and stretches the electrophysiological acumen of a cardiologist, more than a strip of wide QRS tachycardia. Here is a patient who comes with palpitations, with mild hypotension , still comfortably entering the OPD with a non-emergency appointment.
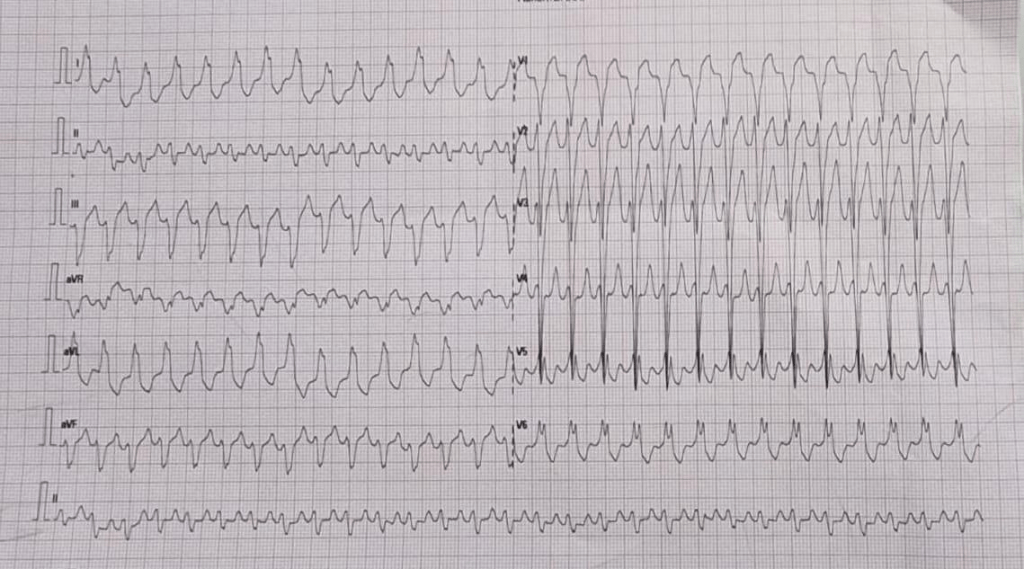
How many diagnosis are running through your mind when you see this ECG . How much it got narrowed after applying criteria like Brugada, Vereckei etc ( VT, FT, OTVT, Mahaim Tachycardia, AVRT /AVNRT with aberrancy etc)
Now let me reveal the age of the patient .He is a 13 year old boy. Does this help you to narrow down the list of possibilities ? Logically, It should , but for some it can widen the list as well .( Brugada, Anderson, Long QT, Naxos all runs through the mind)
What happed next ?
As the cardiologist was wondering how to tackle this arrhythmia . Adenosine? Amiodarone or DC shock, thankfully, the boy got to spontaneous sinus rhythm .
Click here to see the ECG after restored sinus rhythm & the diagnosis is Instant .
Yes it is a WPW substrate. Localization of pathway is a must and a headache for the fellows. .For me, It looks like a posterior pathway in the para-spetal area. 90% of AVRT are narrow QRS . Here it is wide. Why ?
It’s simple. The tachycardia is anti-dromic.
Is it ? Look at the strip again and confirm is this antidromic ?
I am not sure , I still think it is still antidromic .
I am saying No. This is Ortho-dromic wide QRS tachycardia .
How do you say so ?
Antidromic will still more wide and rapid and won’t terminate spontaneously .Of course one problem here aberrancy usually take an RBBB morphology.
How are you so sure . Let us send this to an EP guy.
*What did the EP say? Well, he didn’t commit to anything as I expected. He said until he measures the refractory period of the accessory path, he won’t comment anything about ortho or antidromic query of AVRT. He asked us to send the case for ablation immediately,
Ok. Let us analyse the reason for orthodromic wide QRS AVRT
1.Rate dependent aberrancy
2.Functional abberancy.
3.Preexisting BBB
4.If patients are on drugs that can prolong his Purkinje conduction
Final message
Two lessons may be learnt.
Lesson 1: Trying to decode a wide QRS tachycardia, without knowing clinical background, should be forbidden. This topic is intentionally made complicated by a flawed teaching methodology of wide QRS tachycardia for over 4 decades. Maybe the single lead AVR algorithm promises to be a quick remedy. If AVR is positive, it is VT; cannot be SVT.
(For the curious readers , please go through Dr. Masood Akhtar’s article from Wisconsin on how to differentiate VT & SVT without even looking at the ECG by law of statistics that beat the invasive EP studies).
Lesson 2 : Wide QRS AVRT is not always antidromic . In fact, orthodromic wide QRS AVRT is 2 to 3 times more common. Many of us don’t realise this bias in our learning.
Related topic
How common is orthodromic wide QRS atrial fibrillation ?
Reference
Acknowledgemt
The ECG is posted with courtesy of my colleague Dr. C.Moorthy, Cardiologist, Chennai.
Posted in Uncategorized | Tagged accessory pathway, adenosine test in wide qrs tachycardia, antii dromic vs orthodromic avrt, avnrt vs avrt, avr criteria, broad qrs tachycardia, brugada, fascicualr tachycardia, mahim tachycardia, pre excitation syndrome, rvot lvot vt], vereckei, wide qrs tachycardia, wpw syndrome |
In a country fighting hard to lower its maternal mortality ratio (MMR), one might imagine a clear cut focus on fundamentals like anemia, hemorrhage, sepsis, obstructed labor. But instead, a new fad has crept into antenatal care, camouflaged as progressive medicine. It is the routine ordering of maternal echocardiograms in all pregnant women, a trend that appears to be driven less by evidence and more by fear, peer pressure, and the increasingly fashionable distrust of clinical acumen.
Pregnancy is not a cardiac disease. In fact, most young Indian women undergoing childbirth are remarkably resilient physiologically. But, thanks to a few well-publicized tragic outcomes in heart disease in general media and a rising paranoia, we now find ourselves in the midst of an echocardiographic epidemic, fueled by cardiologists, who are unwilling to say “no” to obstetricians who are terrified of missing something. Lastly, we have a system that forgets that over-testing could penalize patients in a variety of ways.
A spade is a spade whether you like it or not. The average Indian obstetrician today is not ordering an echocardiogram because she believes the woman has cardiac disease. She’s doing it because if anything anything goes wrong, she doesn’t want to be blamed for not “having ruled out everything.” In other words, to protect themselves, not the patients. This is classic defensive medicine, induced by aggressive audits of maternal deaths. What was meant to improve care has blunted our common sense. Government monitoring maternal deaths, though well-intentioned, has induced a culture of cover up obstetrics. When outcomes are uncertain and punitive audits loom large, “Do an echo” becomes the safest default.
But this anxiety-driven medicine is not safe. It’s perfect example of ignorance wrapped in a bag of fear. It is sad to note that even experienced obstetricians refer apparently normal pregnant women for routine echo. More curiously some of them are meant to rule out peripartum cardiomyopathy at 24-30 weeks. It sidelines clinical judgment and turns antenatal care into a tick-box ritual. It transforms even highly skilled obstetricians into a panic referral mode. And all the while, cardiologists, many of whom have seemingly disconnected to stethoscopes, happily oblige. (I used to tease my classmate colleague obstetrician, if you really want to rule out PPCM, you need to do serial echoes at least two, one in term and the next after delivery.)
An echocardiogram costs roughly ₹2000 (or even more) in India today. Multiply that by 2.6 crore annual deliveries in India, and you arrive at a staggering ₹5200 crore annually, potentially spent on an investigation that is not recommended as routine by any global guideline, including those from the American College of Obstetricians and Gynecologists (ACOG), the Royal College of Obstetricians and Gynaecologists (RCOG), or WHO.
However, in India, where we are still battling basic issues like iron deficiency, safe delivery practices, and institutional access to labor rooms, many of the obstetricians are casually considering routine echocardiograms as a screening test in pregnant women. That’s not progressive medicine. (*It must be made clear, there are no official guideline that prescribes routine echo in India, but the obstetrician level trend is worrying.)
Let us not underestimate the psychological cost. A vague or equivocal echo report (mild chamber dilation, trace pericardial effusion, mild gradients creates unnecessary anxiety, referrals, and sometimes even unwarranted interventions. These aren’t just academic problems .They can unleash a cascade of referrals, expensive cardiology consults, prolonged hospitalizations fear-induced C-sections, all in women who never need it. Not to forget the worst of all side effects , the fear. A woman who walked into the antenatal clinic smiling, now spends her nights Googling mitral valve prolapse.
We forget that every test carries the burden of interpretation. And in the absence of clinical suspicion, these echoes do more harm than good. They confuse, they mislead, and they medicalize a natural physiological process.
The Misplaced Narrative: Is Cardiovascular Disease the New Villain?
There is a disproportionate narrative emerging in the corridors of public health, that cardiovascular causes are now the leading cause of maternal mortality. Though this is not entirely false, cardiac causes are rising in urban, high-risk populations. But this narrative, when extrapolated to the entire pan Indian obstetric population, is misleading. Most of these studies are from tertiary referral centers, which jack up the true incidence of heart disease in the general pregant population.
Let’s not forget, biggest killers of pregnant Indian women remain postpartum hemorrhage, sepsis, anemia, and eclampsia. These are not fancy diseases. They are diseases of neglect, of systemic failure, of poor infrastructure. Trying to divert funds, resources, manpower, and policy focus from these core issues toward a speculative cardiac screening agenda is not just unscientific, can be unethical too.
This total dependence on Echo probe, by cardiologists also exposes a deeper malaise. It is the loss of confidence in clinical medicine. Ask yourself, when was the last time a cardiologist palpated a pregnant woman’s apex beat or auscultated thoroughly before performing an echo?
Echocardiography is indeed a quick, non-invasive, accurate tool . We think, there’s little downside for doing it. But this culture is eroding clinical skills. It raises the fundamental question. Have cardiologists lost the confidence to diagnose (or rule out) even simple heart disease without an echocardiogram? This loss of clinical finesse is not just tragic , it is dangerous. It inflates the false positive rate, undermines interdisciplinary trust, and sends the message that technology trumps clinical judgment. It doesn’t.
It is time, we stepped back and asked: what exactly are we doing? Why are we medicalizing normal pregnancy in the name of caution? Why are we spending precious public funds on routine Echo Imaging, when rural PHCs still lack blood banks and partography. Health policy in a country like India must be built on the twin pillars of evidence and equity. Routine Echo fails in both. It is not recommended by global societies, and it redirects attention from more pressing priorities. The answer to maternal mortality does not lie in a Doppler probe. It lies in blood transfusion protocols, nutrition programs, skilled birth attendants, and systemic accountability.
What if if we miss a condition ?
Most young Indian women undergoing childbirth are remarkably resilient physiologically. Even if a minor cardiac anomaly is missed on clinical examination, it rarely alters the course of a normal pregnancy. Ironically, even when we cardiologists do detect such conditions, say, a small ASD or a benign valve lesion we usually end up doing nothing more than “observe” throughout the pregnancy. So the real question is: why are we spending time, money, and emotional burden to look for what we’re not going to treat anyway? Of course, echo is a must in all tertiary hospitals, where high-risk pregnancies are treated.
To the Ministry of Health: Please do not be carried away by the seduction of technology. Focus on the basics. Improve the undergraduate education, with a complete overhaul of the curriculum and arrest the shaky clinical foundation. Build safe spaces for childbirth, increase paramedical workers, and establish a speedy referral system. Don’t fall for universal screening of pregnant women with costly gadgets.
To the Federation of Obstetricians: Have courage. Do not let fear dictate your protocols. Stand for rational care, and reclaim your clinical space. Refer pregnant women for a cardiologist opinion, only if you strongly suspect heart disease.
To our esteemed cardiologists: First, spend sufficient time listening to the pregant women , and then therr heart through the Laennec’s device. Record an ECG. 9.5/10 times you can rule out any significant heart disease. If you decide to do an Echo, ensure it’s truly beyond your clinical sense. I know, the reality is much more troubling. Often times, In India, pregnant women are referred to our office only for Echo, they are least bothered about your opinion. (Why I am saying this, because I had a nasty experience with an Anesthetist-Obstetrician combo, who sort of violently argued with me when i said echo is not required in one particular patient. Their concern was, how on earth, I could certify a pregnant women’s heart as normal without doing an Echo.)
To the public : Remember that not everything that can be tested needs to be tested. Sometimes, the best care is less care but delivered with wisdom.
Final message
Indian pregnant women needs true care out of passion, not out of fear. (Which can lead to cascade of inappropriate investigations) Let us go back to the basics and bring down the MMR with mindful allotment of resources, cost rationalization, and technology worthiness assessment.
Post amble
* Please note : None of the guidelines recommend echocardiography as a routine tool in low-risk pregnancies. All support clinical risk assessment first.
Posted in Uncategorized | Tagged routine echocardiography in pregnant women, screening echo in pregnant women |