Stent scaffolds are supposed to match the natural size of the coronary artery. Cardiologists take a lot of effort to match stent size and vessel wall. Choosing the optimal size, both width and length, is the foundational parameter. However, there is no perfect match possible with the extent of the lesion.
While stent length mismatch is much more common and taken less seriously,diameter mismatch can be more problematic since it looks strikingly odd & ugly .Still, one section of cardiologists believes a little amount of oversizing is safe and good. There is equal opposition to this concept as well. It is not surprising , acquired stent-ectasia of coronary artery during PCI ,has both advantages as well as troubling issues.
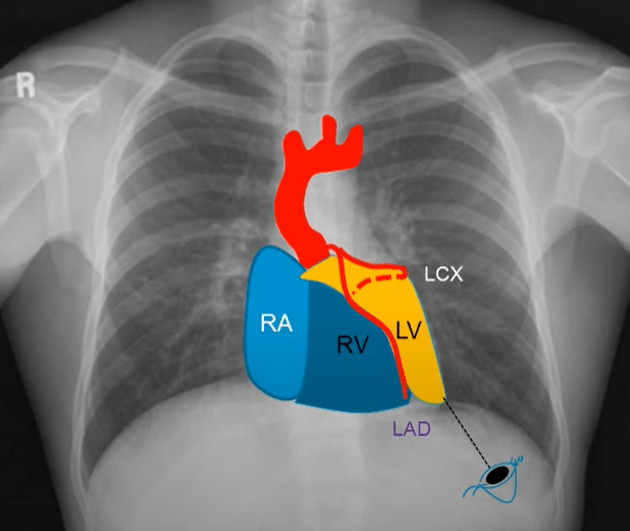
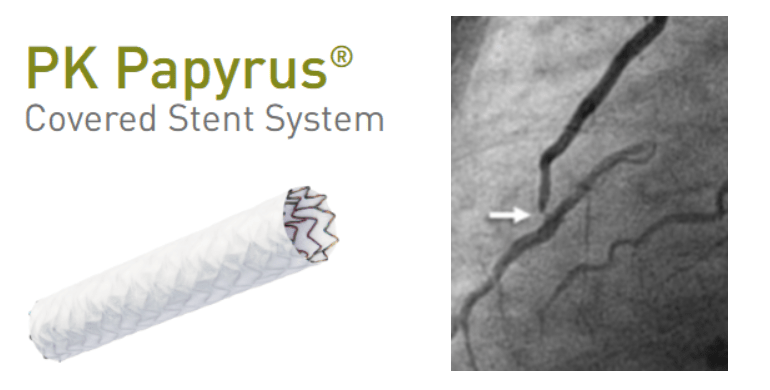
Please note the (?intentional) proximal LAD pythonisation , by oversizing the stent , which provides more lumen reserve area. What are cost and benefits of this bad principles in PCI practice ? Read below
Advantages of Stent Oversizing
Better Apposition and Expansion
Oversizing can ensure full contact between the stent struts and vessel wall, especially in moderately calcified lesions, reducing malapposition. Prevents stent under-expansion, which is a known predictor of restenosis and thrombosis.
Improved Flow Dynamics
Slight oversizing may restore vessel diameter more completely, improving luminal flow and reducing turbulence.
Reduced Risk of Stent Edge Dissection(in selected cases)
If stent is properly deployed and well apposed, oversizing slightly may prevent gaps at the edges where dissection can initiate.
Helpful in Plaque Compression
Facilitates better plaque redistribution and compression, especially in fibro-calcific lesions.
Disadvantages of Oversizing
Risk of Vessel Injury or Perforation : A stent that is too large can overstretch the vessel, causing deep medial injury, dissection, or even perforation especially in fragile vessels or older patients.
Increased Elastic Recoil : Oversized stents in small or elastic vessels (e.g., RCA) may provoke recoil, paradoxically reducing the luminal gain.
Edge Dissections and Geographic Miss : If oversizing leads to excessive radial force at edges, it can cause edge dissections, especially if not well matched with tapering vessel anatomy.
Neoatherosclerosis and Late Malapposition : Chronic vessel injury from over-expansion may lead to inflammatory changes and promote neo-atherosclerosis, stent fracture, or late acquired malapposition.
Stent Fracture Risk : Over-expansion of certain stent platforms beyond their elastic range increases risk of metal fatigue and fracture, especially in tortuous or mobile segments.
Final message
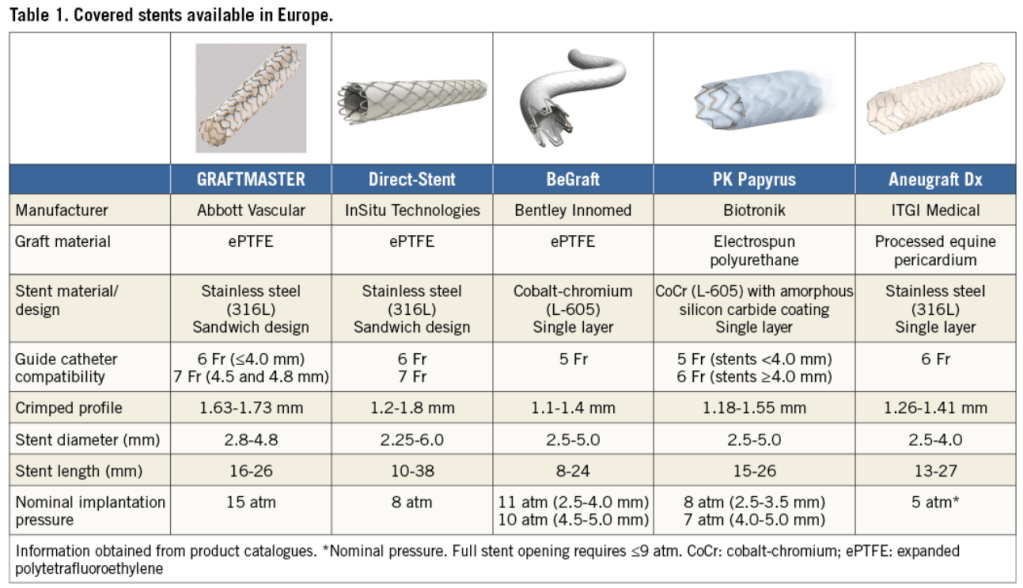
De novo coronary ectasia is quite a common and fairly benign entity seen in 20 to 30% of normal coronary arteries. However, acquired ectasia (stent-ectasia) can’t be taken lightly. No one can predict who is going to accrue the potential benefit and risk. Slight oversizing of stents (typically within 0.5 mm above reference vessel diameter) can be beneficial in selected clinical situations, such as in fibrotic or calcific lesions, or in large proximal segments. However, it must be done cautiously, guided by imaging (IVUS or OCT), and never exceed the manufacturer’s recommended expansion limits.
Reference
This IVUS-based study on nearly 3,000 lesions found that slight stent oversizing (within 0.5 mm of reference diameter) led to better stent expansion and lower restenosis, without increasing complications.
This landmark randomized trial (IVUS-XPL) showed that IVUS-guided stent sizing often resulting in slightly larger stent selection and greater expansion reduced major adverse cardiac events significantly at 1 and 3 years.
Post-amble
Can we do an intentional post-dilatation to increase the lumen size in small vessels ?