Some times I wished, I could have become a Nephrologist. This thought comes whenever we face a patient with unexplained dyspnea, normal EF, and heart size. Am I missing a HFpEF? The heart is not like the kidney, which injects the all too familiar BUN & creatinine into blood promptly (with a high degree of reliability). Even a medical neophyte can diagnose renal failure just like that.
Cardiologists don’t have that luxury. Of course, we do have NT-Pro BNP recently , which nowhere comes near to renal failure markers . Still, many of the youngsters are tuned to believe NT-Pro BNP is equivalent to creatinine for the heart. Remember, biochemical diagnosis is always an adjunct and never confirmatory This is because NT-Pro BNP is universal cardiac stretch molecule , that can elevate in big list of conditions. Similarly , to appear in the blood, there can be a time lag unlike creatinine. (Read the universal definition of heart failure below).
* Though , a key link word and /or is used widely, unfortunately , the definition fails to reiterate clinical signs will prevail over biochemistry at any given point of time. It has inadvertantly ? given some over wiegtage to biochemistry.
Also, the new definition has gotten rid of hemodynamic, metabolic, and chamber-wise RV, LV classification systems. I think the committee wanted to remove the clutter of terms. In a broad sense, it’s good. By using the word structural, it includes valve defects or pericardial pathology into the basket of HF.
Now getting deeper, can we differentiate differentiate HFpEF from HFrEF, based on biochemical markers ?
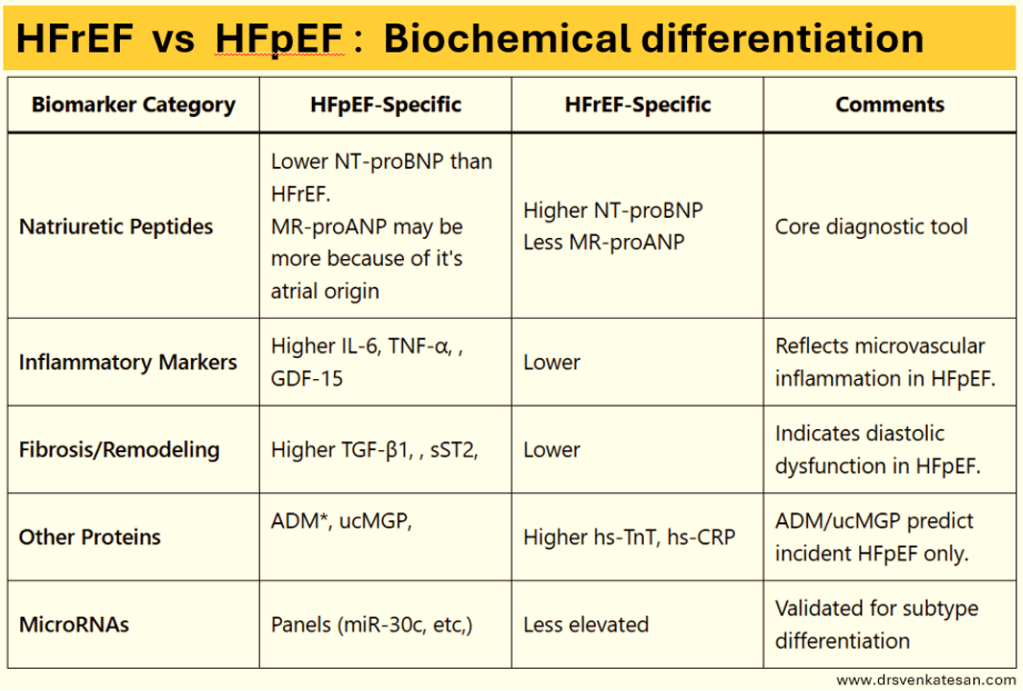
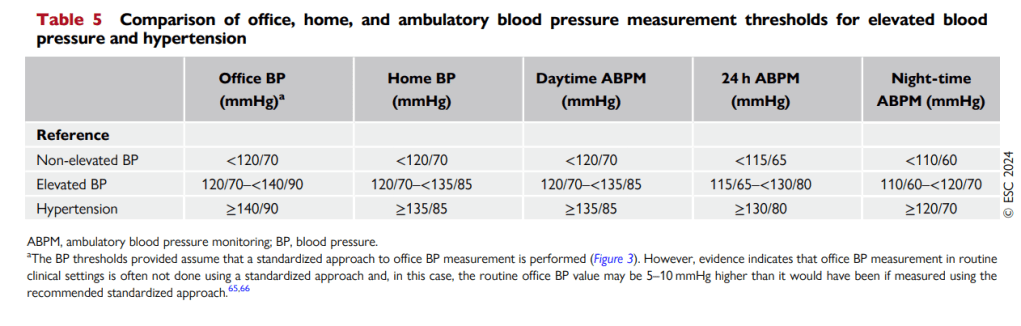
Differentiating HFpEF and HFrEF is vital but looks complex. One may say it is not really complex. Funnily , the purpose of the above chart becomes redundant if the EF of 50% has already differentiated the two conditions . what is the big deal about this table ? It is purely for prognostic and etiological purposes.
Summary
NT-proBNP is typically lower in HFpEF due to reduced ventricular wall stress, while MR-proANP which originates in the atria are expected to be more in HFpEF . Inflammatory and fibrotic markers and MicroRNA panels are high and more specific to HFpEF.
*Growth differentiation factor-15 . **ADM -Adrenomedulin a biomarker for arterial stiffness and arterial calcification . ***ucMGP refers Uncarboxylated Matrix Gla Protein. MGP to function as a calcification inhibitor,
Final message
Recognizing and confirming HFpEF, itself can be considered a partial clinical success. (Since more often it is missed) As mentioned earlier, biochemical differentiation is largely an academic exercise but gives us an idea of systemic pro-inflammatory and local fibrotic status.
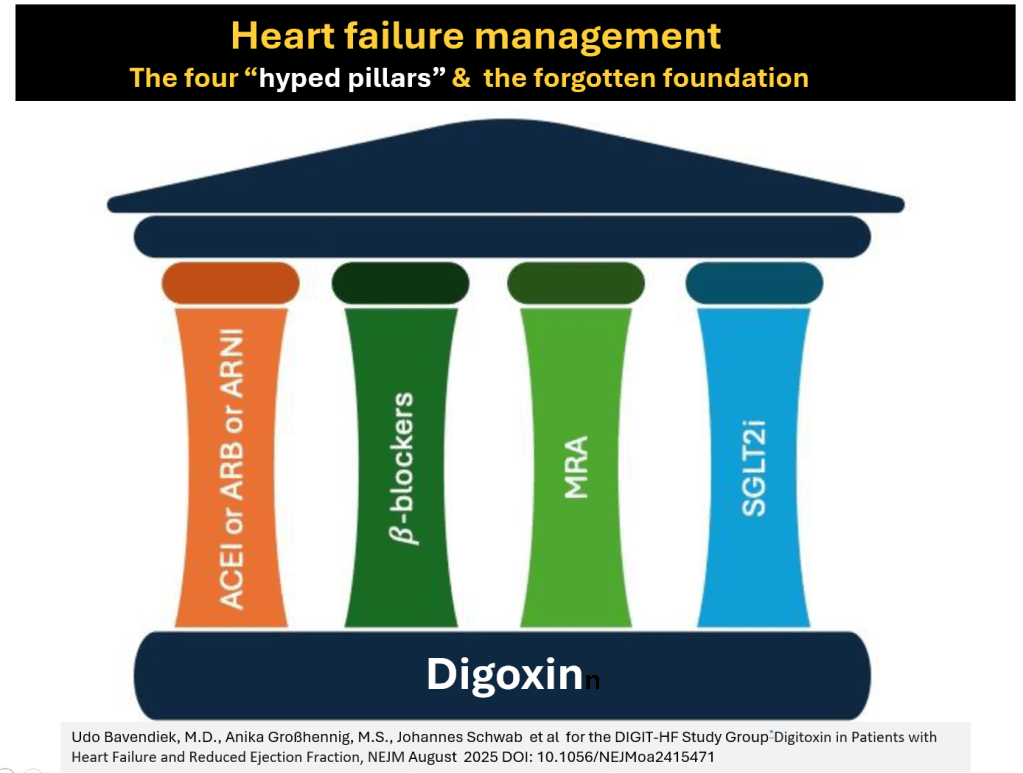
There is a rough pathological rule of thumb (Note the word rough again). HFpEF is more often a systemic condition where the heart is affected. (In contrast to HFrEF where the pathology of the heart is central, and all systemic features are secondary to it.) Treatment options for heart failure have improved overall .However it is more limited in HFpEF as Inotropic agents are redundant here. Prognosis is highly variable and not necessarily better.
Reference
1.Ho JE, Lyass A, Lee DS, et al. Circulating biomarkers of incident heart failure with preserved ejection fraction: the ARIC study. JAMA Cardiol. 2018;3(5):415-423.
2.Zile MR, Desantis SM, Baldauff N, et al. Biomarker-guided risk assessment for the diagnosis and treatment of heart failure with reduced ejection fraction and preserved ejection fraction. JACC Heart Fail. 2021;9(12):893-903.
For Fellows . How do you diagnose HFpEF ?
- Clinical features of heart failure (Apply some criteria , ex-Framingham )
- Some evidence of elevated LV filling pressure at rest or exercise (Diastolic stress test)
- Normal LVEF > 50% (Must ensure this should not be a recovered and improved EF from HFrEF condition)
- NT-ProBNP -Supportive