Stents have become essential coronary jewelry in global CAD care. The usage of these glamorous metals inside the human heart has crossed many millions, and aiming for a billion. Obviously, when used on such a large scale un-toward events are not an exception.
Stent migration
While the complication list of coronary stenting hangs long, fortunately, stent migration is a rare event. , Though, early geographical miss is common during deployment, these episodes don’t come under stent migration. Stent dislodgement during the procedure is a more common technical defect.If not recognized it may be wrongly labeled as late migration Exaggerated longitudinal shortening sometimes mimics migration.
Minor stent skids or mini migrations in cath labs are acceptable, distant and wayward migration to dangerous zones can be problematic.

True migration may be defined as a stent moving away from the target zone in the short or long term from its original location. It is useful and can be further divided with reference to time like peri procedural, short term, and late. Though it is generally thought to be rare true Incidence is not known. (Colkesen AY, . Int Heart J. 2007;48(2):129–136.)
Mechanism
It is not always easy to find the reason for migration. Many of the following factors could operate
- It is tempting to blame the technique, inappropriate size (small for the lumen), and lack of imaging whenever migration occurs.(Very often one of them is true)
- Metallurgically, it is the radial strength that keeps a stent in its original place. if for some reason this force is lost there is potential for migration of the stent. In this context, there is a link between stent fracture, injury infection, and migration of the stent.
- A vasospastic coronary artery holding the stent tight and later releasing the grip is a rare possibility.
- Liberal use of vasodilators like nitroglycerine might contribute. A case report from Pakistan suggests this possibility Murat Celik, Pak J Med Sci. 2013
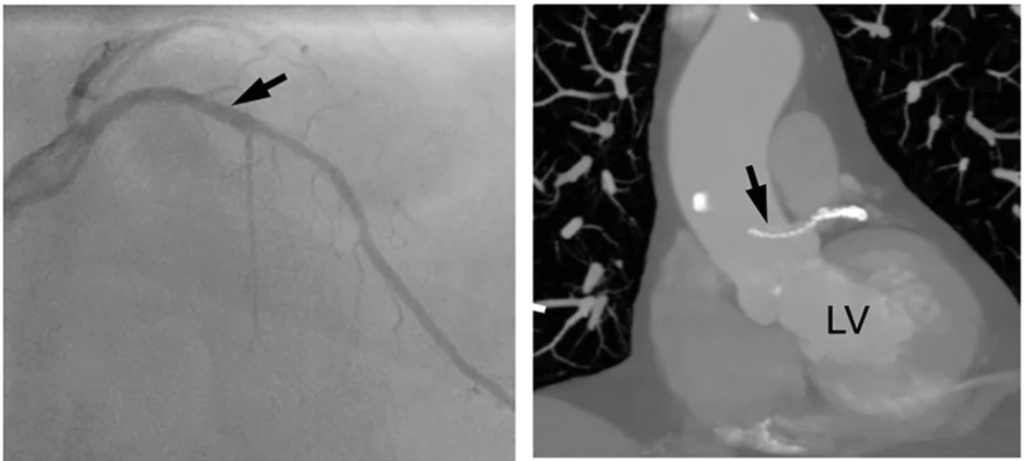
- The coronary artery is not a static tube so is the stent . the artery can milk out foreign bodies if it wishes. Fortunately, it doesn’t. Instead, it reacts with metal and initiates an inflammatory and rejection process that may ultimately end up as infective aneurysm and the stent can migrate outwards or extraluminal into the aneurysm sac. We realize, this is more common than other forms of migration.
- Retrograde migration is a baffling complication as in the following case.
Implication
Stent migration can be totally unrecognized by many, while could end with a dramatic clinical event depending upon the extent and location of migration.
Extraluminal migration into pericardial space has been reported. Praloy Chakraborty, J Am Coll Cardiol Case Rep. 2021 May, 3 (5) 745–746
How do we manage this?
Though it is a sort of crisis for cardiologists, very often patients are asymptomatic and comfortable in spite of migration. (After all, it is the same pro-thrombotic foreign body even if it is present in its original place, is it not ?) Minor migration or embolization to safe zones need not require any intervention.
What should we do if leaving alone is not an option?
Crossing the stent and deploying it again or trapping or crushing it with another stent or retrieval are various options. Surgery is the last resort if the migrated stent is compromising blood flow critically.
Stent migration: A mini ethical crisis
Should we inform the patient about this adverse event?
Never hide any info from your patient about his or her health. It may amount to serious negligence. Sorry, I beg to differ*. If we really feel, it is a safe migration, and if the patient’s (& relatives) anxiety is too high, principles of practice of medicine can be selectively put on hold, for the overall benefit of the patient. (Of course, legal requirements are to be fulfilled by documenting the event in a complex manner as the lawyers do )
*Once you inform the patient, the option of leaving it unattended is a Herculean task even if it’s benign migration. (at least in our country) We have had long debates about this. Once upon a time, we had a stent that got dislodged and lost in circulation, and after long times of screening, there was a suggestion of a stent in the pelvic branches of the iliac artery. I will leave to your imagination, what we did for that patient.
Final message
Stents have conquered our profession and it is a life-sustaining device for both patients and cardiologists. Along with it, we have percutaneous valves, wires ,plugs, disc conduits, ICDs etc, Welcome to the big world of vascular foreign bodies. We are supposed to get optimally trained to keep all this stuff within the circulatory system smoothly running. If you look in that perspective, stent migration may be considered a minuscule untoward event. This doesn’t mean we can take this entity casually. We need to be familiar with its true incidence, mechanisms, potential solutions, and preventive strategies.
Reference
1.Bews and others, Coronary stent on the move, European Heart Journal – Case Reports, Volume 5, Issue 12, December 2021, ytab511, https://doi.org/10.1093/ehjcr/ytab511
2.Kasegaonkar AM, Chudgar P, Kamat N, Burkule N, Dhareshwar J, Dalal A. Delayed Presentation of Intracoronary Stent Migration in Pericardial Space: Role of Imaging. Indian Journal of Clinical Cardiology. 2022;3(4):209-210. doi:10.1177/26324636221087108



