We keep doing RCT after RCT trying to find out the truth, whether opening CTOs are really useful. Meanwhile, cardiologists continue to do CTO- PCI as per their wishes, convenience, and perception of the literature.
5 major studies are available about the utility of PCI in CTO
It seems, it is far easier to do multiple, multicenter RCTs than to interpret the findings of these trial results. However , we have mastered the art of tunnelling down blindly, both in the ante & retro grade routes , tackling the tortuous and often rocky, CTO terrains and complete a wonderful PCI. Still, we are not sure ,whether it is worth all the efforts and risk ?
What does it mean? It conveys a simple truth. Our hands work more brilliantly than the brains.
video source and courtesy https://asahi-inteccusa-medical.com/asahi-inteccs-interventional-microcatheter-guide/
Studies on CTO
A.EURO-CTO
B.COMET-CTO
C.IMPACTOR-CTO,
D.DECISON CTO
Of the above four, only the DECSION -CTO was negative, still many cardiologists are not ok to do a CTO PCI . Why ? The reason is simple. They know the truth that, none of trials showed improvement in overall survival .
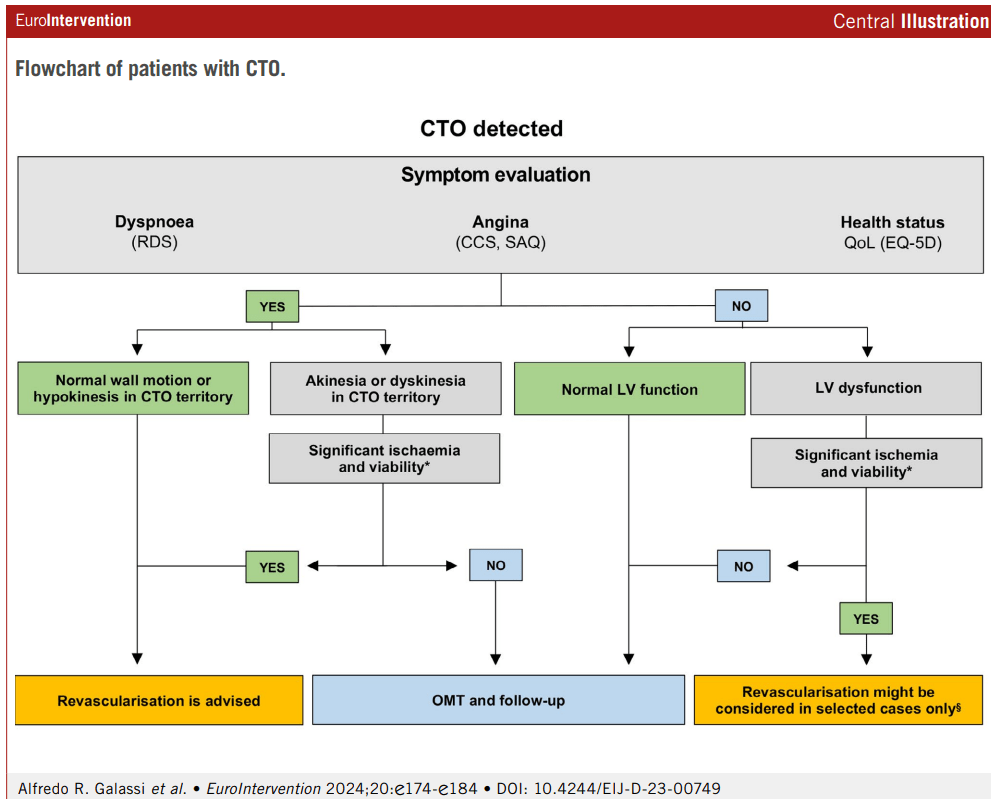
Most studies looked only at angina as a symptom .Very few included patients with dyspnea as a symptom . While it is rare to recruit asymptomatic patients in clinical trials, in real world it do happen very often, ie getting rid of the block as an indication .
We do get some useful information from these trials
1.Expertise and hardware .We have good technology to do a successful PCI .
2.Don’t open it just because you do it
3..Simple documentation of viability is not enough. We have top prove the same viable segment is critically ischemic as well .The buck doesn’t stop there, the procedure we do should be good enough to eliminate that ischemia ,
4.If symptoms are angina and it is refractory, one may consider CTO PCI. Never do it for relief of dyspnea, even if the guidelines suggest you to do so.
When can do a PCI in CTO without guilt ?
We do have official algorithm
CTO procedure deftly improves both cardiologist’s’ & patient’s sense of well-being, provided the patient doesn’t experience any complications, which can be anything between 3 to 20%.
Why Indication for CTO PCI are still tentative and vague ?
*We are yet to do a proper study addressing all the important variables in the CTO pathology and hemodynamics.
*Even if, we do a good study , they are not properly interpreted.
*Even if it is properly interpreted, guideline writing committees tend to be biased towards more action than inaction.
*It is strange ,Inaction (not doing a PCI) is seen as a therapeutic defeat for a cardiologist as he leaves a patient, who has a blocked coronary artery, however healthy he may be.
Conclusion
If we are not able to arrive at a meaningful conclusion even after many RCTs on the on the same topic ,what does it mean?
It could mean only one thing. Studies and trials are not the real answer to the questions which we are asking .There is something more we have to look at. Mathematics and biology can’t be fused as we desire.
Reference