Hi, welcome Mr George, I just reviewed your records. You have three blocks in your arteries supplying the heart.
Are they serious Doctor ?
Not really, but one of them appear tight
What should I do Doctor ? But, I am comfortable Doctor.
You may be. But I am not .You need to undergo some re-vascularisation procedure .
What do you mean by that Doctor ?
It means either a percutaneous coronary intervention with a stent or CABG.
Can I get my heart re-vascularised by drugs alone Doctor ?
No we can’t . Hmmm , wait, we do have something called OMT/GDMT. Can you put on hold for some time Mr George, you have asked a real tough question.Let me recollect something from my forgotten basics clinical lessons.
The Illusion of myocardial re-vascularisation
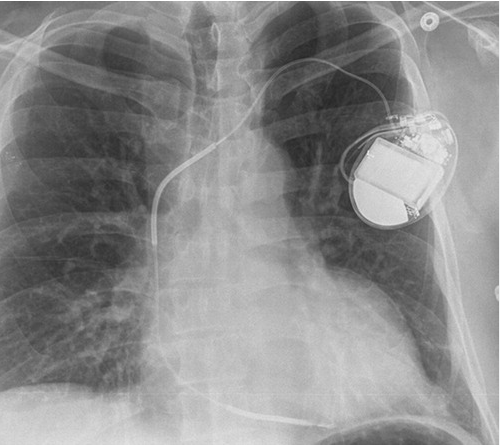
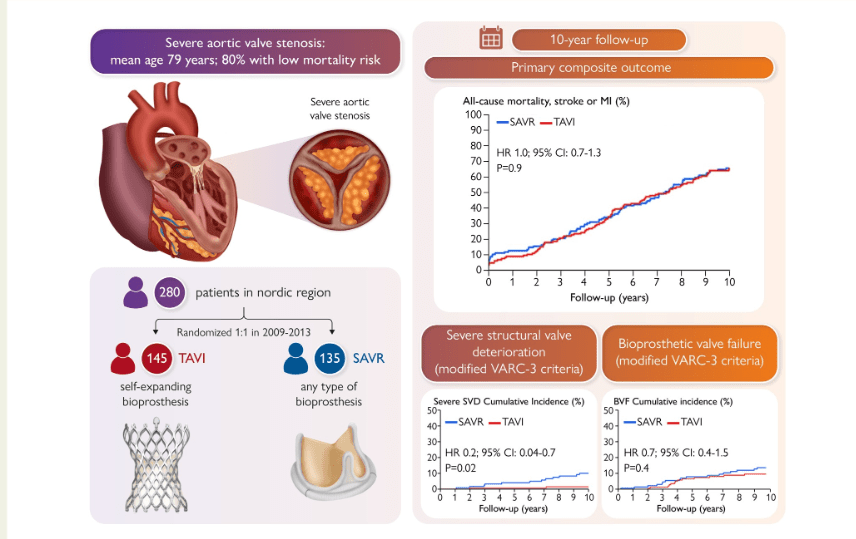
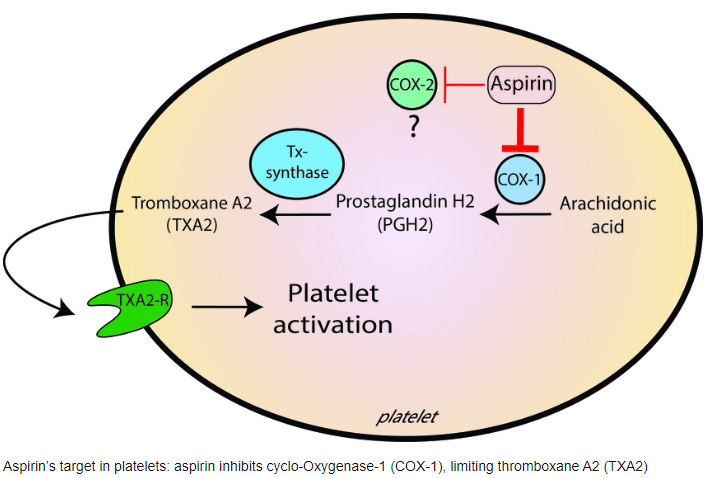
PTCA is sort of repair work done over the blocked area that restores the traffic(blood) flow. while CABG, diverts flow from the congestion or road closure, along a by- pass road, which rejoin the main road later. These are called re-vascularisation procedures. Please note, both of them, never bother to find the status of micro-vascular integrity which form 95% of net coronary vascular surface area.
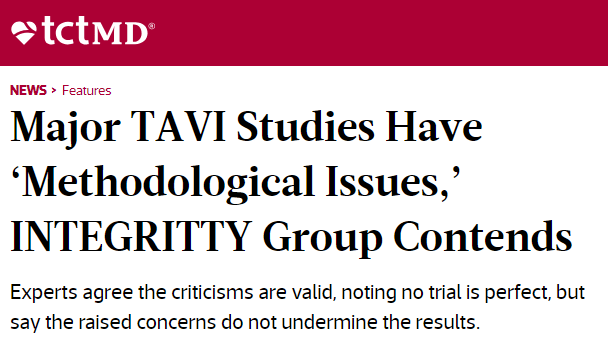
Hiding behind the technicalities
PCI demands reduction in percentage stenosis , resulting in pre-defined minimal luminal area (MLA), maximizing net luminal gain, & restoration of TIMI 3 flow in all three coronary arteries .These are the popular scientific parameters. For CABG we aim at good and complete, uninterrupted short and long term distal flow.
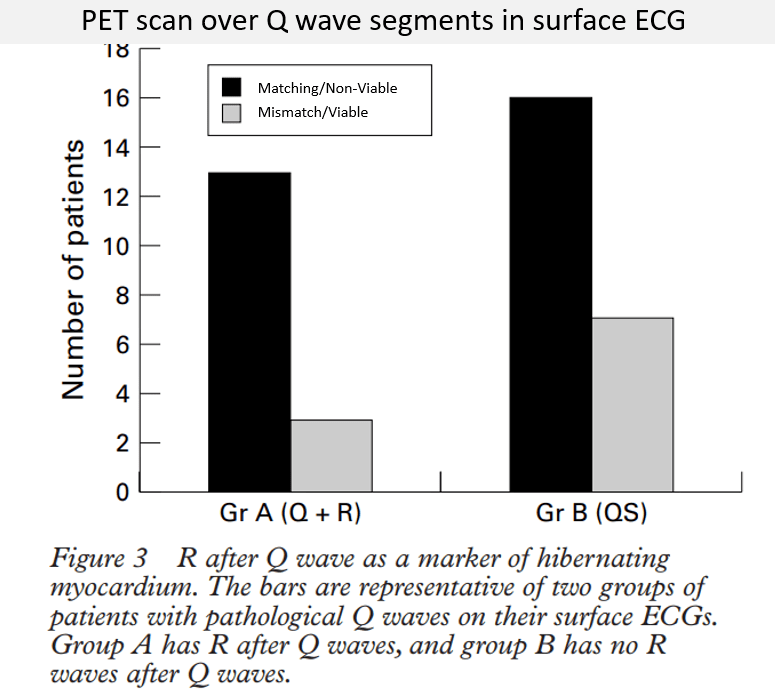
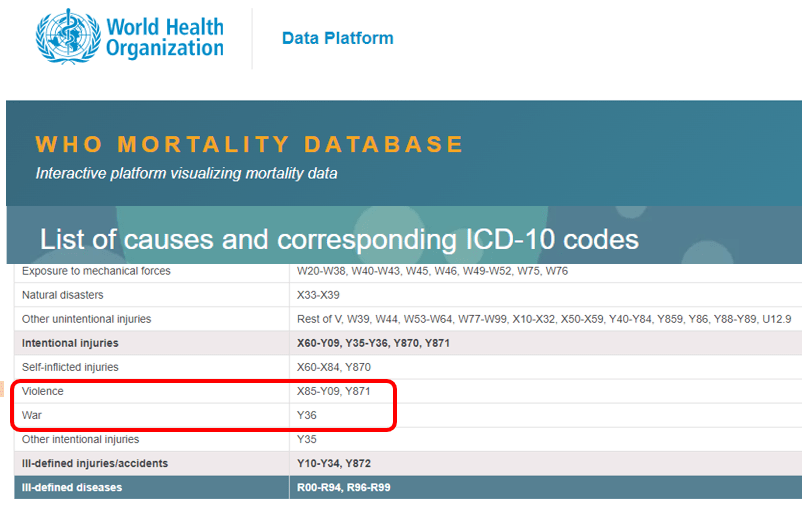
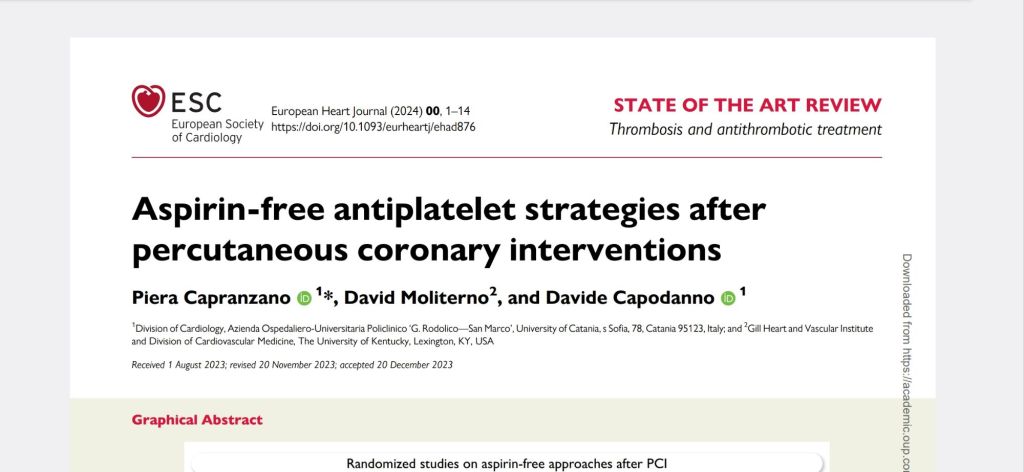
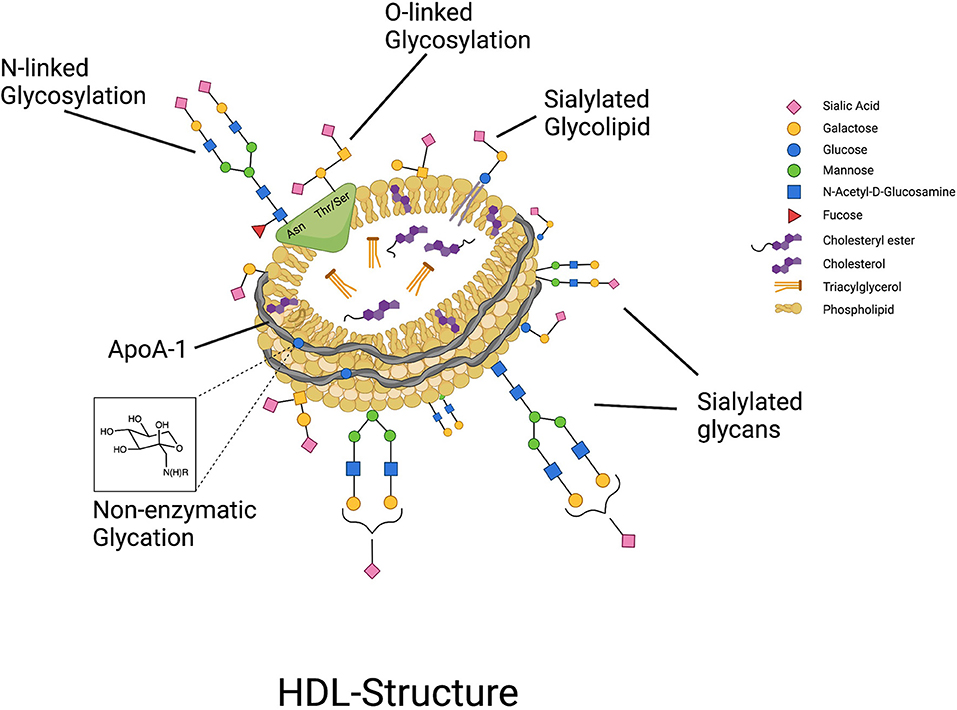
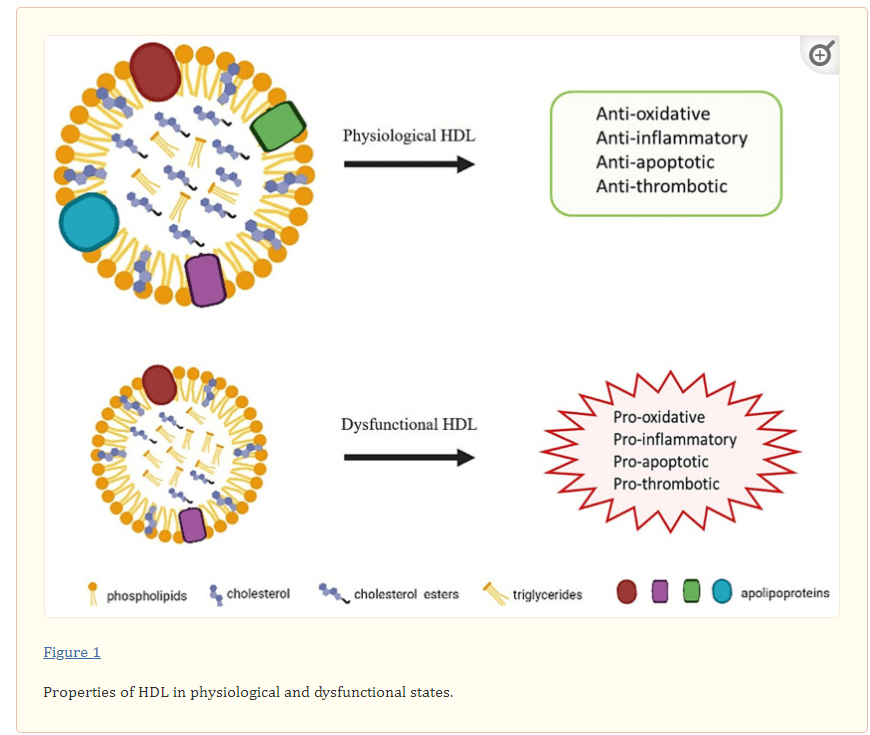
However ,we have some effective clinical and pathological markers too, for effective re-vascularisation They are clinical well being and good functional capacity , relief from chest-pain, reduction of plaque volume, plaque stabilisation, maintenance of collaterals , microvascular patency , reduction of recurrent events .The irony in CAD management is in many patients who are on only drugs , clinical endpoints can be achieved without the above mentioned technical end points ! ( As we have learnt from the OAT, COURAGE trials which dramatically showed arterial patency is nothing or little to do with major clinical end points )
Final message
Scientific minds can not accept certain things which are less glamorous and unassuming. Simply swallowing few drugs can never make us(both physicians and patients) believe it can be an equivalent to PCI/CABG .
Intentionally or unintentionally , we have made PCI and CABG appear invincible and conferred the sole-rights to be referred to as re-vascularsation procedures , Realistically looking medical therapy also provide good revascualrisation (re-or neo) especially where it is needed ie in the coronary micro circulation.
Hence forth, in the overall interest of CAD community , and with good scientific basis “It is good to emphasise to our patients optimal medical management of CAD is also one form of re-vascularization This will help us to neutralise the unfair” Semantic advantage” the PCI and CABG enjoys.
Reference : Apart from the heavily quoted classics of COURAGE, BARI-2D, ISCHEMIA, ORBITA 1 etc. (Please note ORBITA -2 is not an antidote to ORBITA-1) ,Read this 1.AVERT study :Atorvastatin equals PCI .2.Regular exercise equivalent to PCI (ESC 2009) .Will try to get the link for this soon.