History beckons… once upon a time, assessing severity in valvular heart disease was gloriously simple. We used to just a pullback pressure gradient across the aortic valve . Now, history repeats itself, as the same philosophy returns to coronary arteries, offering a surprisingly elegant solution amid a chaos of physiological indices. That is PPG .
What Is PPG*?
Pullback Pressure Gradient (PPG) is a physiological mapping method that evaluates the pressure gradient across a coronary artery using a gradual pullback of a pressure wire . It helps to:
- Localize ischemia
- Differentiate focal from diffuse disease
- Guide a more logical PCI strategy
Rather than a strict binary verdict (ischemic or not), PPG gives us a gradient map — revealing how pressure falls, where it falls, and whether intervention makes sense.
*I would love to call it as plain old PPG. POPP-G . (Sort of POBA equivalent in PCI)
How to Measure It ?
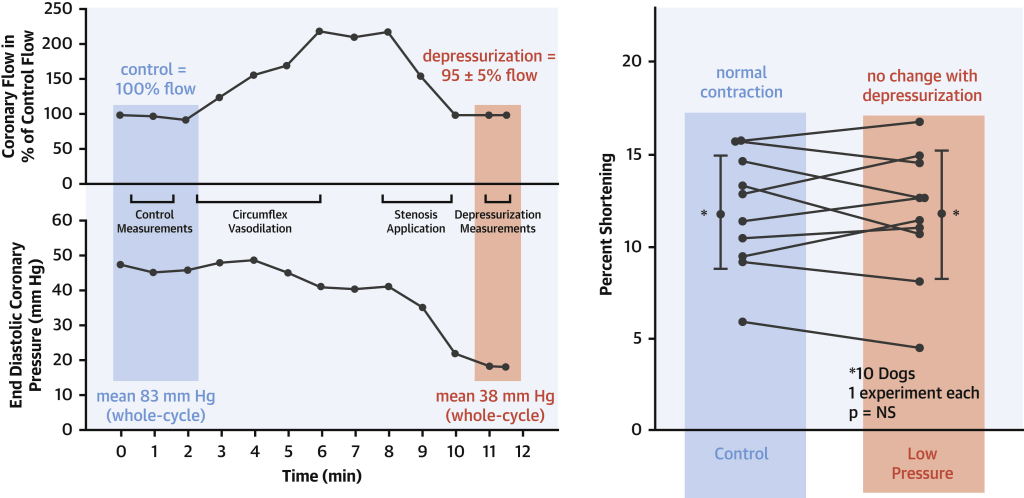
- Essentially it is a less glorified iFR or FFR .Same hard ware is used.
- Pull back happens in both .But ,here thats is only that happens, that’s devoid of the clumsy Adenosine protocols, Incomplete hyperemia, patient anxiety, or microvascular dysfunction etc.
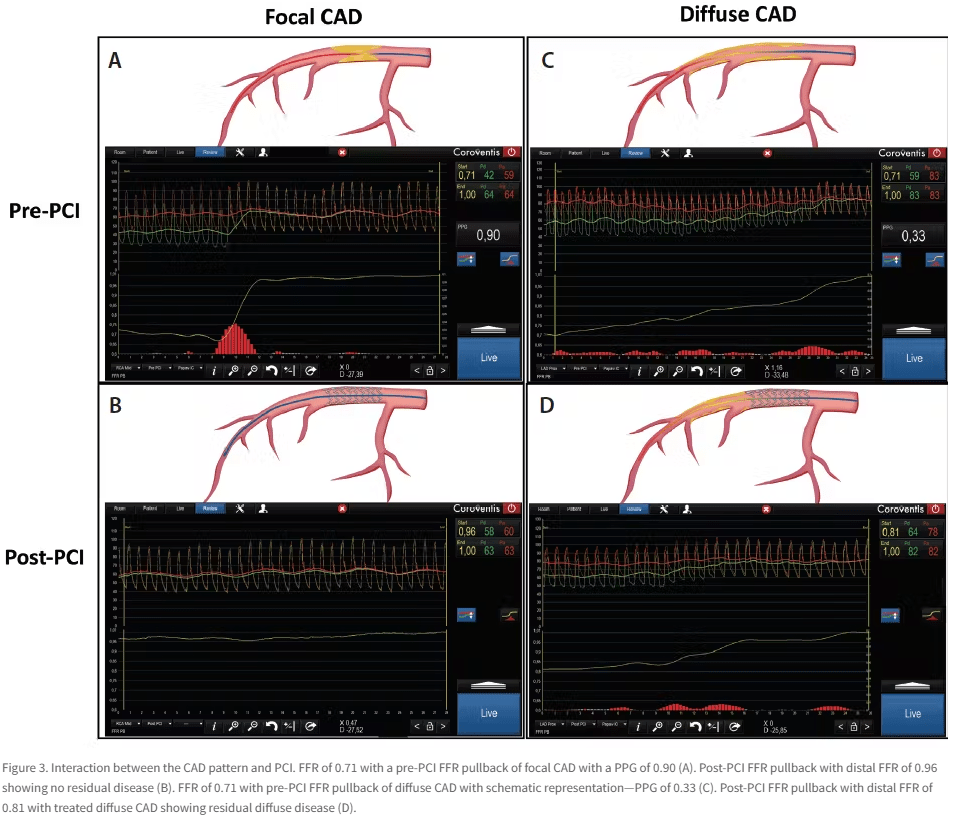
- Apart from measurinng pressure drop the rate of fall the gradient slope is also analysed. PPG = ΔP / pullback distance (mm) .If the slope is steep the lesion is probably stentable . If the rate of fall is slow or flat we may avoid stenting.
PPG is a dynamic, localized, gradient-based insight into coronary disease. A focal ΔP over small length ΔL would be a perfect PCI candidate. A flat gradient over long ΔL , would suggest medical therapy .(May be CABG in few)
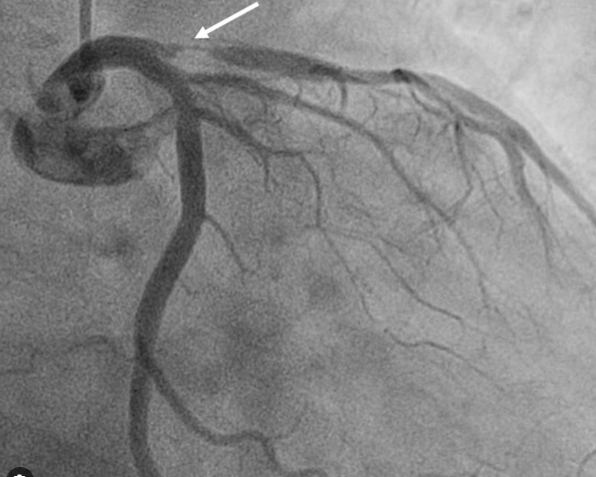
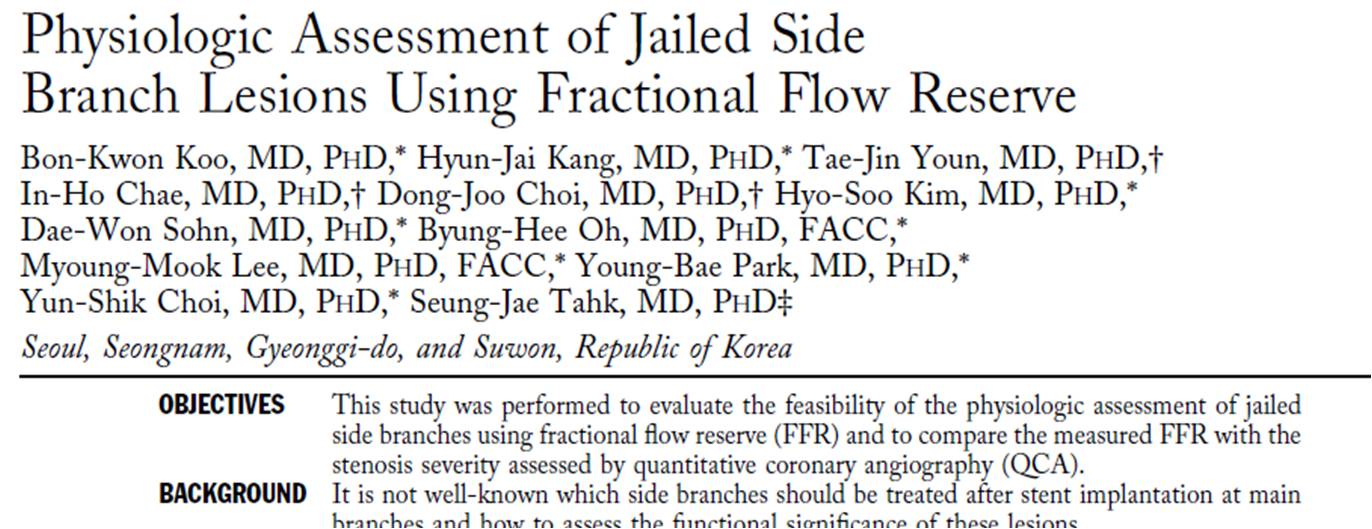
PPG in bifurcation Lesions
How do you FFR in bifurcation or trifurcation lesions . If you ask this question to any cardiologist, will try to get away from the scene. Such is the complexity involved. Here comes the savior. PPG helps you out in a smart fashion.
- PPG allows branch-specific physiological localization, Can be used selectively in each branch to map the true pressure loss. This is contrast to the crude FFR that may falsely elevate due to competitive flow or tandem disease.
- PPG can avoid the unnecessary double stenting and of course make the make the bifurcation club members unhappy in the process. PPG also can help detect ostial branch disease (by inching technique we do in cardiac auscultation,) by very slow pull back.
Image courtesy : Daniel Munhoz CARDIAC INTERVENTIONS TODAY MAY/JUNE 2021 VOL. 15, NO. 3
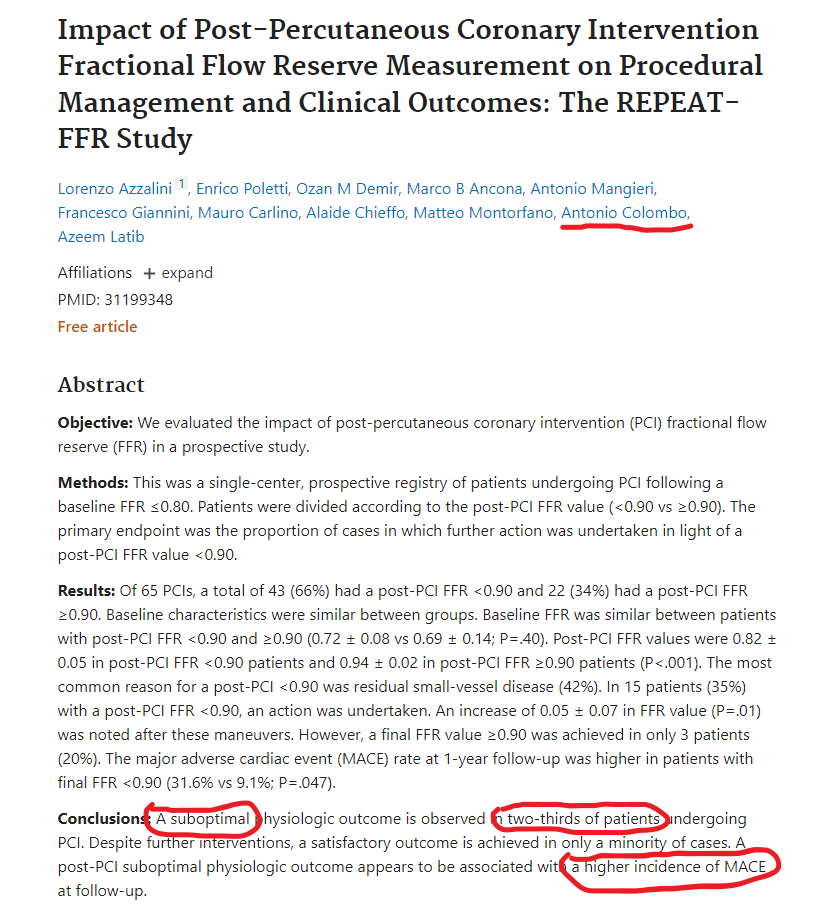
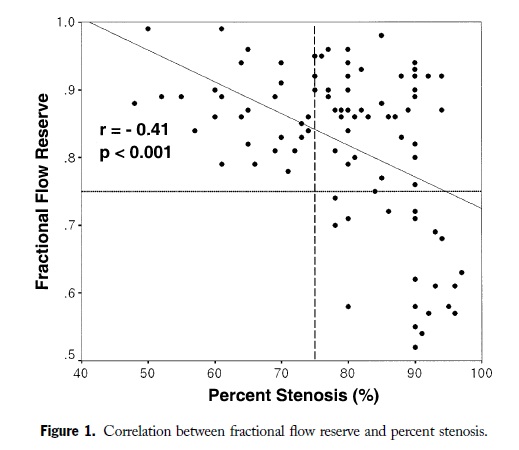
Is FFR really problematic ? Be aware of conflicting studies
FFR was a great concept when it came in. FAME I study adored It. FAME II questioned PCI’s benefit despite FFR-positive lesions. Then came DEFINE-FLAIR and iFR-SWEDEHEART, questioning the need for hyperemia at all. Still, residual ischemia post-PCI in up to 20% of cases (DEFINE-PCI) even when FFR said “normal.” Confused? So are most cardiologists.
Modern cardiologist’s dilemma: How to cross coronary jungle infested multiple flow Indices ?
The list is long . FFR , iFR, FFR-CT, QFR, RFR, dPR, NHPR, µQFR (there are few more I might have left ) . None are perfect. Some contradict. Some cost too much. Many need drugs. All add layers of complexity to what should be a simple clinical question: Should I stent this lesion? Now, we have the simple plain PPG.
Why should, we fall for PPG ?
Let’s be honest. PPG is not flawless. After all, we take pressure drop as a surrogate marker for restricted flow . Every Indices does that. But unlike other indices It’s intuitive. It’s visual. It tells you where to treat. It gets the pressure data on the spot from ground zero . It can bring reliable info without the need for intracoronary medication , or costly software. Finally, it restores some simple sense in us ,without great knowledge in coronary hemodynamics.
Reference
- Kobayashi Y, Johnson NP, et al. “Physiological Assessment of Residual Ischemia After Coronary Stent Implantation Using Instantaneous Wave-Free Ratio.” JACC Cardiovasc Interv. 2019;12(19):1996–2007. https://doi.org/10.1016/j.jcin.2019.04.040
PPG-based residual gradients predicted poor outcomes post-PCI even when angiographic results looked fine. - Collet C, et al. “Stress myocardial perfusion imaging vs coronary functional assessment with PPG and FFR: A physiologic map approach.” Eur Heart J. 2021;42(10):926–938.
PPG superior in identifying focal lesions amenable to PCI compared to binary FFR thresholds. - van Belle E, et al. “DEFINE-PCI: Residual Ischemia Post-PCI Detected by PPG and iFR Pullback.” JACC Cardiovasc Interv. 2019;12(20):1991–2001.
Post-PCI ischemia often missed by angiography alone — PPG reveals it. - Davies JE, et al. “Use of the Instantaneous Wave-Free Ratio or Fractional Flow Reserve in PCI.” N Engl J Med. 2017;376:1824–34.
iFR non-inferior to FFR .Suggests resting physiology-based PPG.