Cardiogenic shock (CS)is the most feared event following STEMI. The incidence is up to 5 to 10% with a mortality rate of around 50-60%. Still, we are finding it hard to bring this down below 50 % .There is one less addressed issue in ACS literature. We tend to perceive CS as an exclusive complication of STEMI. The fact is that NSTEMI can also result in CS is less recognized. The incidence is half of that of STEMI, i.e., 2.5-5%.
Mechanism of CS in NSTEMI
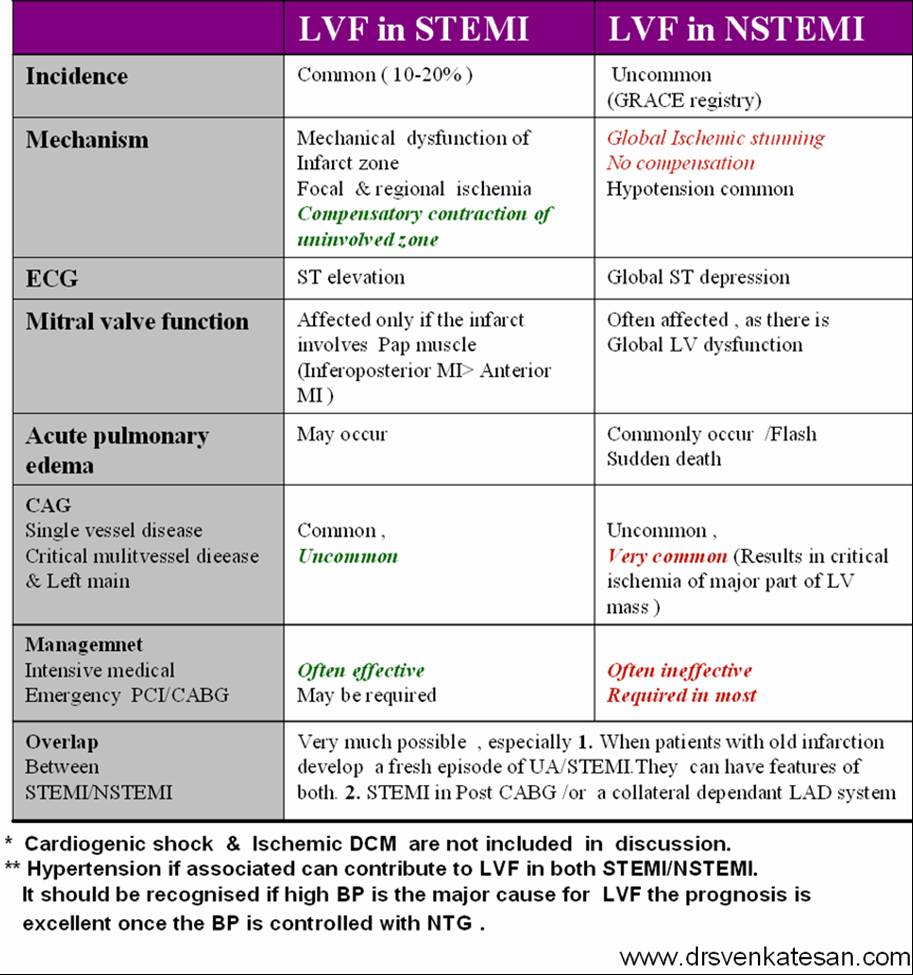
One may ask, how can CS occur in NSTEMI with partial occlusion with a non trans-mural MI. ACS pathophysiology is not that simple. Ischemic LV dysfunction (Global stunning) without necrosis is equally sinister. This is what happens in some high risk sub sets of NSTEMI.
How is CS in NSTEMI different ?
1.Global ST depression (AVR.V1 might show little elevation with considerable overlap of left main STEMI vs NSTEMI )
2.Onset of NSTEMI-CS occurs late (48-72 hrs)
3.Severe multivessel disease is more common (It is likely ,presence fold STEMI , is an important factor that is likely to precipitate CS when a new NSTEMI occurs.
4.Echo is likely to show more of a Global hypokinesia rather than specific coronary territory
5.Mechanical complication, though less common in NSTEMI , Ischemic MR especially with LCX- NSTEMI can be problematic and much commoner than we think.
6. A subset of NSTEMI precipitated by acute severe HT and flash pulmonary edema has excellent prognosis if BP is reduced promptly. (This can be simply a equivalent of HT, with no true supply side ischemia with LVF with global ST depression )
Management
*More or less similar to STEMI with aggressive opening of culprit lesions with few differences. (unlike STEMI, CULPRIT SHOCK trial doesn’t apply here )
*May require CABG more often
*Mechanical circulatory support will be needed in many
*Finally, and importantly, there is more likelihood of systemic factors like sepsis, Anemia, or renal or kidney failure contributing to the CS in NSTEMI than STEMI. In fact, we have observed pre-existing HFpEF can be a contributory factor.
Outcome
There are differing data about prognosis of CS in STEMI vs NSTEMI. Early mortality is higher with STEMI; but, late mortality converges. Ironically, in many patients of CS in NSTEMI, the outcome can be worse than STEMI, as there is no single culprit and myocardial salvage does not appear to be a primary issue. (Ref 2)
What does SCAI guideline say about CS in NSTEMI?
Nothing, yes it is true. Are you surprised ? A search for the word NSTEMI in both these document drew a blank. May I kindly request SCAI team to look in this, CS in NSTEMI deserve better recognition in their guidelines at least in their next edition (Ref 3,4)
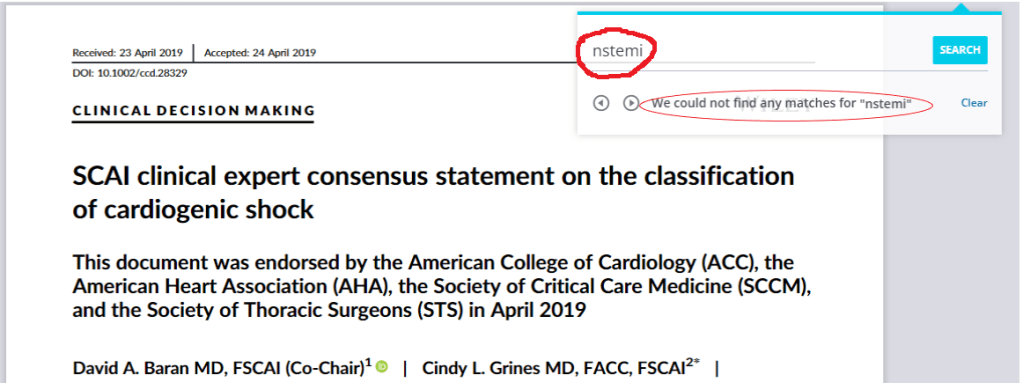
I am not sure why SCAI classification didn’t address CS in NSTEMI as a separate entity.
Final message
Surprisingly , CS in NSTEMI is not a well researched entity in cardiology literature. Fellows are requested to analyse the GRACE registry once again or create their own institutional experience.
Reference