A young women with Rheumatic heart disease .
Mitral regurgitation is significant .www.drsvenkatesan.com
When do you call a left atrium as giant ? When it is referred to as Aneurysmal dilatation ?
It is all semantics. Whenever LA becomes more than 6 cm , at least in two diameters many prefer to call it giant .
In India , 6 cm LA is such a common finding , we have kept a cut off at an arbitrary 9 cm .
What factors determine a LA to dilate like a balloon ?
The exact mechanism is not known.It could be the intrinsic weakness of LA wall , as very few with RHD develop this. Many LAs resists dilatation even in the midst of extreme LA pressure. But , it is a well-known fact , mitral regurgitation provokes greater LA dilatation than MS alone .This implies volumetrics play a major role than pressure dynamics in determining LA size. Acuteness of hemodynamic insult is inversely proportional to LA size.
By the way, what is the purpose of recognizing the LA as Aneurysmal ?
- In plain X -ray chest , LA may form the right heart border over shooting the RA.
- When LA becomes huge , there is a chance for mechanical complications like dysphagia, phrenic nerve , bronchial compression etc .
- Giant LA invariably increases the chance of LA clot.
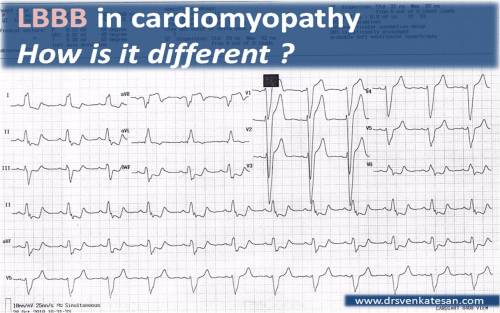
Electro-physiological Issues
- Atrial fibrillation , a usual accompaniment of giant LA , is often refractory . There is no purpose to convert to sinus rhythm . In fact , one should not attempt this. There was a time when surgical incisions ,corridors , mazes were quiet popular.Now it is believed all these are adding further injury to the ill-fated LA .Electro-physiologists should be restrained . Pulmonary vein ablation should never be attempted in such cases as the focus of AF is elsewhere .
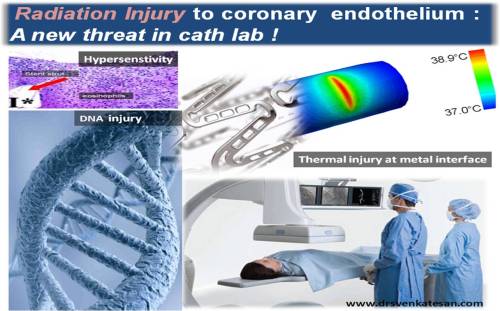
Implication in cath lab
During PTMC LA size can be an issue as the plane of IAS is distorted and make things difficult for septal puncture . Further the balloon , guidewire may often slip back into RA .
Implication for the surgeon.
For the surgeon the implication could be more. As a cardiologist I can’t comment about that .One thing we have observed is when LA becomes huge , the size of mitral annulus is too fictitious and funnily enough we have recorded up to 6 cm of mitral annulus . No valve is available for this size . We learnt from the surgeons , large LA rarely pose a problem as they suture the much smaller valve in a larger annulus .(Which makes the task that easier )
Does the LA size regress after surgery ?
In many it does regress , in as many it doesn’t. We have seen giant LAs continuing to trouble the patient even after a successful mitral valve replacement.
Read Full Post »