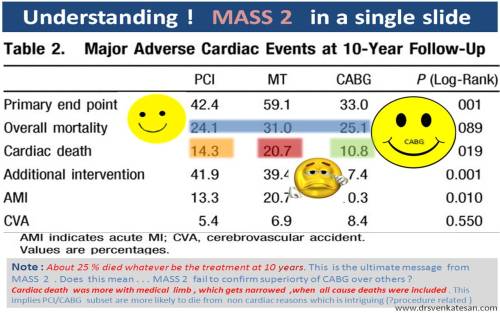
MASS 2 study , the 10 year follow-up results are just out in circulation september 2010 .
It is a rare study , where “one to one vs one” was compared ie the effect of medical, CABG , and PCI in chronic CAD .This was done in a single centre in Brazil, between 1995 -2000 . It was followed up till 2010. Interestingly , such a study may not be possible in the future , as many of us have prematurely glorified the PCI and CABG over medical therapy . Recruiting patients for medical therapy alone is becoming a difficult job even in developing countries. Even if we recruit , huge cross over is likely to PCI, CABG for all fancy reasons.
So , in MASS 2 we have a rare treasure on hand . . . Let us give three cheers to those Brazilians who did this study , and shall carefully analyse and interpret the results.
Highlights ( According to my interpretation)
- A total of about 600 patients with 200 in each group.
- The overall death at 10 years is not greatly different . (Around 25 % )
- But ,cardiac deaths were distinctly higher by few percentages in pure medical arm
- Need for crossover from medical to surgery and PCI to surgery was significant.
CABG tended to prevent future MI in this study . This could be most significant observation from this study ,( A revelation in fact ! ).It is against the popular belief created by CASS legacy.
What are the observed difference between MASS 2 – 5 year results , which was published in 2004 , and the 10 year follow-up , as on 2010 ?
At the end of 5 years in 2004 , the differences among the three groups were not obvious.The benefits of CABG mainly appeared after the 5th year and at 10 years it was significant.
Shortcoming of MASS 2
- It is a single centre study .Numbers were less (600) .
- It need to be emphasised CABG was done with pump in all patients . So the currently prevalent off pump CABG may not be really comparable with reference to outcome.
- Only bare metal stents were used in PCI .(If only DES was used . . . Considering the host of issues for and against DES , it will be a wild guess to judge it’s implication . It could have tilted , either in favor or against the PCI limb .)
- In medical limb , statins were not used in all. Further , the dose of statins were not aggressive.This makes medical therapy appear less effective.
Intriguing thoughts
When we say medical therapy is being compared with PCI and surgery , we are actually comparing ,
Medical therapy alone
Medical therapy+ PCI
Medical therapy + CABG .
Every patient in all three groups receive statin , antiplatelet and beta blocking drugs and so on. Even though statistics would vouch for additional benefit , over and above medical therapy , in a given CABG individual , how much of the the accrued benefit is contributed by co- administering medical therapy .It is beyond reasoning even with all gimmicks of statistics.
To exactly quantify the individual benefits and efficiency of PCI , CABG and medical therapy two more study limbs are necessary .
- PCI without drugs.
- CABG without drugs.
Such a study is possible only in a virtual world ! . Decision making in favor of CABG , especially in chronic stable angina , will continue , to be difficult in the absence of refractory angina .This is due to the modest benefit of CABG , that is expected, at an additional risk , cost and expertise.
Please remember, a person can survive , only with medical therapy for > 10 years but no one can ever live with PCI or CABG for that period of time without adjunct drugs . Guess which modality is going to win the race against CAD in the long run ?
Final message
If any one asks for conclusion of MASS 2 study , don’t ever say “CABG is superior to medical therapy” . Please emphasize , “CABG + medical therapy could be , marginally superior to medical therapy alone in some of the patients with chronic stable angina. (Each word in the above statement is important !) .
So . . . MASS 2 : Is it a shot in the arm or shot in the head for CABG , we do not know !
http://circ.ahajournals.org/cgi/content/abstract/122/10/949
http://circ.ahajournals.org/cgi/content/full/122/10/949 .This study was done by Zerbini foundation Brazil