This article is in response to the prevalent belief about primary PCI for STEMI endorsed by world cardiology forums. (Caution: A highly personalized version)
Time window in STEMI
- Is the window half-opened or half closed ?
- Is it open at all ?
- Or ,does it open only for primary PCI ,and tend to close down bluntly for thrombolysis
Modern medicine grew faster than our thoughts .We have witnessed the audacity of advising arm-chair treatment for MI till later half of last century . Now we are talking about air dropping of patients over the cath lab roofs for primary PCI.
Still ,we have not conquered the STEMI. While , we have learnt to “defy death” in many patients with cardiogenic shock , we continue to lose patients(“Invite death “) in some innocuous forms of ACS due to procedural complications and inappropriate ( rather ignorant !) case selection.
Note : The ignorance is not in individual physician mind , it is prevalent in the whole cardiology knowledge pool.
The crux of the issue for modern medicine is , how to reduce risk in patients who are at high risk and how not to convert a low risk patient into a high risk patient by the frightening medical gadgets.
In other words , arm chair treatment for STEMI was not (Still it is not !) a dustbin management . It has a potential to save 70 lives out of 100. What many would consider it as , nothing but the natural history of MI .
Medical management of STEMI is ridiculous !
That’s what a section of cardiologists try to project by distorting the already flawed evidence base in cardiology. Some think it is equal to no treatment. Here we fail to realise, even doing none has potential to save 70 lifes out of 100 in STEMI who reach the hospital.
Out of the remaining , 10 lives are saved by aspirin heparin (ISIS 2) and the concept of coronary care . Another 7 lives are saved by thrombolysis (GUSTO,GISSI) . PCI is shown to save saves one more life (PAMI).The remaining 6-7 % will die in CCU irrespective of what we do .
Of course , now medical management has vastly improved since those days . A thrombolysed , heparinsed , aspirinised , stanised with adequately antagonized adrenergic , angiotensin system and a proper coronary care ( That takes care electrical short-circuiting of heart) will score over interventional approach in vast majority of STEMI patients.
Now comes the real challenge . . .
When those 70 patients who are likely to survive , “even a arm-chair treatment“, and the 20 other patients who will do a wonderful recovery with CCU care , enter the cath lab some times in wee hours of morning . . .what happens ?
What are the chances of a patient who would otherwise be saved by an arm-chair treatment be killed by vagaries of cath lab violence ?(With due apologies ,statistics reveal for every competent cath-lab there are at least 10 incompetent ones world over !)
In the parlance of criminology , a hard core criminal may escape from legal or illegal shoot out but an innocent should not die in cross fire , similarly , a cardiogenic shock patient with recurrent VF is afford to lose his life , but it is a major medical crime to lose a simple branch vessel STEMI (PDA,OM,RCA ) to die in the cath lab, whom in all probability would have survived the arm chair treatment.
Why this pessimistic view against primary PCI ?
Yes, because it has potential to save many lives !
Time and again , we have witnessed lose of many lifes in many popular hospitals in India , where a low risk MI was immediately converted to a high risk MI after an primary PCI with number of complications .
I strongly believe I have saved 100s of patients with low risk MIs by not doing for primary PCI in the last two decades.
*The argument that PCI confers better LV function and longterm beneficial effect is also not very convincing for low risk MIs .This will be addressed separately

The demise of comparative efficacy research.
Primary PCI is superior to thrombolysis : It is agreed , it may be fact in academic sense .
Experience has taught us , academics rarely succeeds in the bed side.
“superiority studies can never be equated with comparable efficacy”
Only the questions remain . . .
- Where is comparative efficacy studies in STEMI ?(Read NEJM article )
- Why we have not developed a risk based model when formulating guidelines for primary PCI ?
- Is primary PCI for a PDA /D1/OM infarct worth same as PCI for left main ?
- Is high volume center guarantee best outcomes ?
Who is preventing comparative efficacy studies ?

Primary PCI : Still struggling !
This study from the archives of internal medicine tells us , we are still scratching the tips of iceberg (Iceberg ? or Is it something else ?) of primary PCI

Even a pessimistic approach can be more scientific than a optimistic !
When WHO can be influenzed and make a pseudo emergency pandemic and pharma companies make a quick 10 billion bucks , Realise how easy it is for the smaller , mainstream cardiology literature to be hijacked and contaminated .
Final message
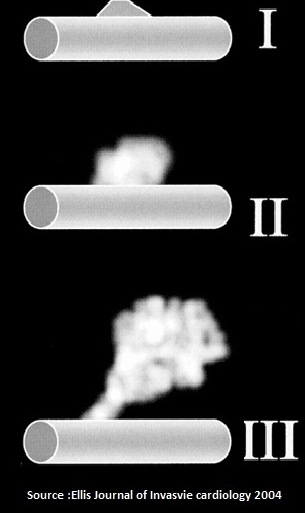
Why we reverently follow the time window for thrombolysis, while we rarely apply it for PCI ? This is triumph of glamor over truth . The open artery hypothesis remains in a hypothetical state with no solid proof for over 2o years since it was proposed.
Apply your mind in every patient , do a conscious decision to either thrombolyse , PCI or none . All the three are equally powerful approaches in tackling a STEMI , depending upon the time they present .Remember , the third modality of therapy comes free of cost !
Never think , just because some one has an access to a sophisticated cath lab 24/7 , has a iberty to overlook the concept of time window !
Remember you can’t resuscitate dead myocytes , however advanced your enthusiasm and interventions are !
Realise , common sense is the most uncommon sense in this hyped up human infested planet.
Read Full Post »