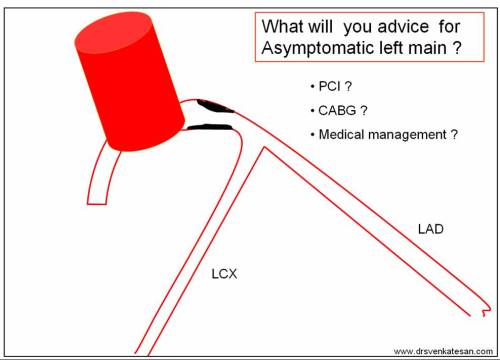
Conquering left main disease is considered as crowning glory for the Interventional cardiologists. For over three decades , CABG has remained the undisputed modality which is being challenged today. Fortunately, the Incidence of true isolated left main disease is low .(If Medina bifurcation subset is excluded)
With growing expertise , advanced hardware and Imaging ( like a 360 degree OCT fly through view ) one can virtually sit inside the left main and complete a PCI .
Still , coronary care is much . . . much . . . more than a technology in transit !
Most importantly, these complex PCIs require rigorous maintenance protocol with meticulous platelet knockout drugs , patient compliance and the genetic fate of drug efficacy . (Clopidogrel has since entered the final laps of inefficiency while Ticagrelor has some more time I guess !)
What is the current thinking about unprotected left main PCI ? Let us know it from real life experts !
For those answered , yes to the above question please leave this page , as the following question might trouble you much !
While competent surgeons are waiting to tackle left main by surgical means ,there are many centers which are Inclined towards PCI though we lack long-term outcome (At least 10 years like CABG )
Why do you think this is happening ? Are you ready for another crooked poll ?!
What exactly is left main disease ?
Some of us also suffer from a knowledge gap and tend to think Bifurcation lesions and left main disease are two distinct entities .The fact of the matter is , significant subset of bifurcation lesions are Indeed either left main equivalents or true left mains ( Medina 1,1,1 would constitute > 50 % all bifurc lesions ) If you include Invisible left main lesions in Medina ( 0,1,1 or 0,0,1 ) detected by IVUS/OCT it might reach easily cross 90% (Scientific guess !) Does that mean we have to think CABG even for all complex bifurcation lesions ? and reserve left main disease for isolated discrete mid shaft or ostial left main ?
Final message
My observation (Sincere to my limited conscience !) at least in this part of the world is : Left main Interventions are “perceived as pride” and its more related to “show of expertise” and is little to do with patient outcome.Unfortunately , cardiologists should not be blamed for it in isolation as the studies they follow are conflicted.
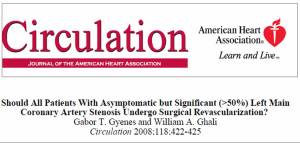
Forget SYNTAX/PRECOMBAT trials, the two famous studies EXCEL (Favor PCI) and NOBLE were published in 2016 made our life tough .One suggested PCI is acceptable /on par with CABG, while the other one put CABG superior , ensuring clarity replaced with confusion ! When we have a dispute , logic would suggest we should fall back on the status quo ie “CABG is superior” unless proved convincingly. Many sections of cardiology society failed to appreciate this.
Post PCI thoughts
*It may not be that hard to do a complex PCI . But, it’s never easier to understand current cardiology literature that is supposed to raise our intellect , which has a direct relevance to patient welfare. Note, many crucial , high stake studies tend to play academic deceit games with linguistic and statistical hyperboles like Non Inferior , likely superiority , Never inferior , near equipoise , regression of hazards, virtual follow-up in real vs trial world etc , etc !
I can only hope for a better scientific world !
Reference
- Which is the best option for left main disease PCI or CABG ? Journal of Individual wisdom and evidence based conscience : Volume 1 Chapter 1- Coronary Intellect : Pages 0 to ∞ Jan 2018.