A. The Aortic Radiologist
B. The Principal operator of TAVI
C. The co-operator or the proctor
D. The device type, behavior & destiny
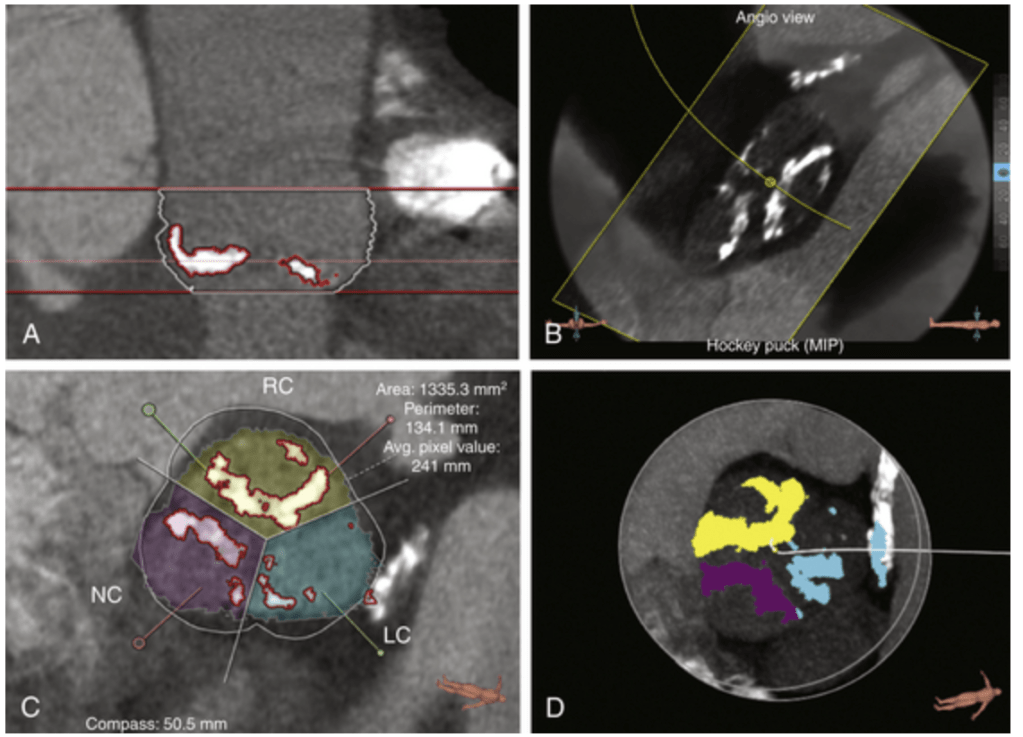
Answer : A. The radiologist, (rather the soft-warist ) tell us best landing zone in the pre procedure work up taking into the account of shape, size, leaflet morphology ,3D analysis of aortic root, and calcium distribution. He plays a vital role. Though B, is the logically correct answer, ie the expertise of the primary Operator it is not to be. Considering the complexity of the anatomy, device, and momentary longitudinal and circumferential alterations in radial forces, In reality, the answer is D.
Evidence? No one has tested so far the true intended landing zone and the final one.
One may argue , the question need to be reframed as, What are the factors that decide the landing zone in TAVI ?
Though deployment is under the control of primary operator , the valve often defies operators’ hand commands and decides to home in its own place of comfort and peace adjusting to the complex anatomy around. It never bothers about the consequences .The unpredictability of calcium crystals, the annular tensile strength, the distorted native leaflet and the blind plastering against the aortic wall all are responsible for the complications. One less talked dynamism of aortic root which finetunes micro adjustments of the valve. Para valvular leak is primarily determined by either excess (or lack )of this modulatory forces.
Following are some of the crucial factors that determine landing zone.
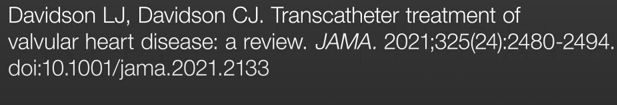
Anatomy of the Aortic root
The ascending aortic curvature and angulation is a major factor of the TAVI landing site. , stretching from the aortic annulus to the proximal ascending aorta. This anatomy may vary depending on the patient and affects different types of valves (such as balloon-expandable or self-expanding). For instance, higher aortic angulation (Ex – a horizontal aorta) can influence the final depth of valve implantation, especially for self-expanding valves with longer stent frames.
The invisible radial & longitudinal forces
The resistance offered by the distorted native valve and its delicate balance with the instant radial force of in case of balloon expandable or the gradual built in force of self expandible balloon system. Apart from the radial forces. the longitudinal deformation forces in long axis as the stent expands , in the last few seconds determine the final residence of the valve.
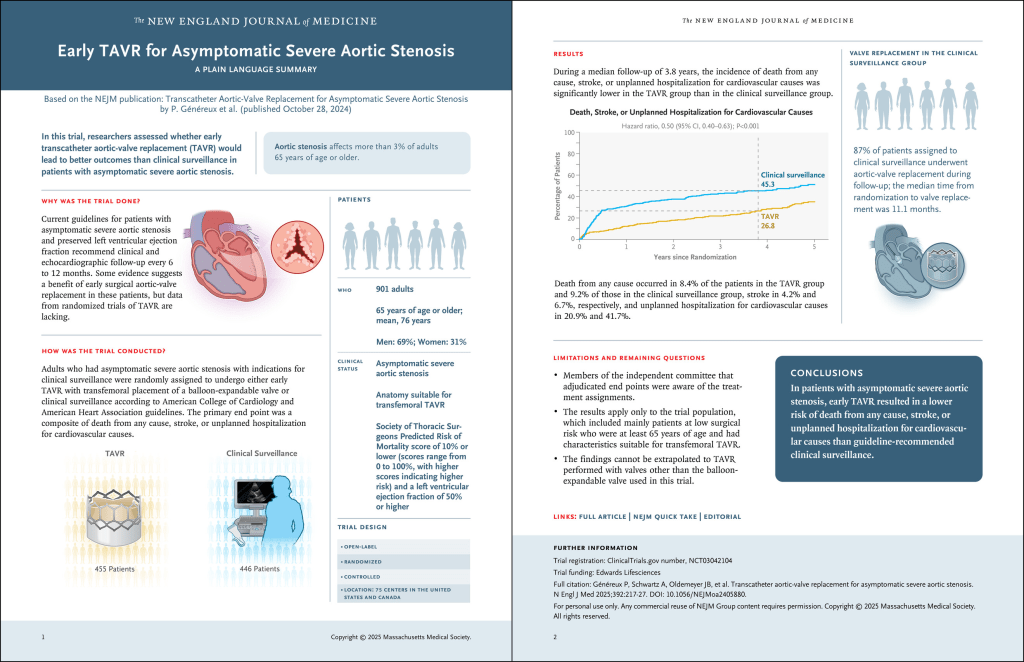
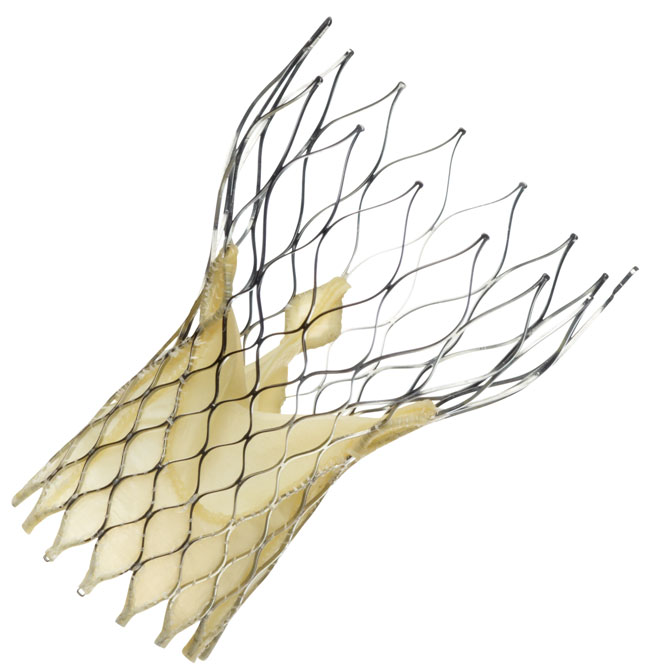
Valve Type and Device Design
The intended implantation depth is usually planned based on the valve type—balloon-expandable valves have a short stent frame and are deployed differently than self-expanding valves with a taller frame. More precision is required in balloon expandable valves. This is because the anchoring mechanisms and the metallurgy is entirely different between the two.(SE-TAVI uses Nitinol frame, and it has wide contact area so more stable ,)
Intra-Procedural Adjustments:
The final landing zone is also influenced by the need to avoid complications such as valve migration, aortic regurgitation, and coronary obstruction.
Final mesage
Some times, TAVI landing looks like SpaceX Dragon docking with a space station. Extreme precision is required to avoid complications. The bulk of the complications are due to inappropriate landing (too high or too low). Fortunately, aortic annulus exists in multiple transverse planes; patients can often tolerate some geographical miss. Still even a few mm error can crash the patient as well as our reputation.
Postamble
What are the chances of immediate post -procedural movement and late migration of the valve from the landing site in TAVI ?
The chances of immediate post-procedural movement and late migration of the valve from the landing site in Transcatheter Aortic Valve Implantation (TAVI) are generally low but represent serious complications when they occur. Incidence is up to 7.5%
Reference
https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2022.928740/full
* Video source and courtesy