It was 2006
Allow me to recount an unassuming piece of a PowerPoint presentation from my institute, Madras Medical College, at the annual Cardiological Society meeting in New Delhi. The paper was categorized under miscellaneous sessions. I vividly remember the day. I have to admit, It was a nearly empty hall E, located in the basement of Hotel Ashoka. After the talk, I looked up to find that neither the chairman nor the handful of kind academic souls had any questions or comments to make. Pausing for a few moments, I quietly walked down the podium with an inexplicable silent pain.
The title of the presentation was “Non-dilated cardiomyopathy”
Welcome to ESC Congress Amsterdam August 2023
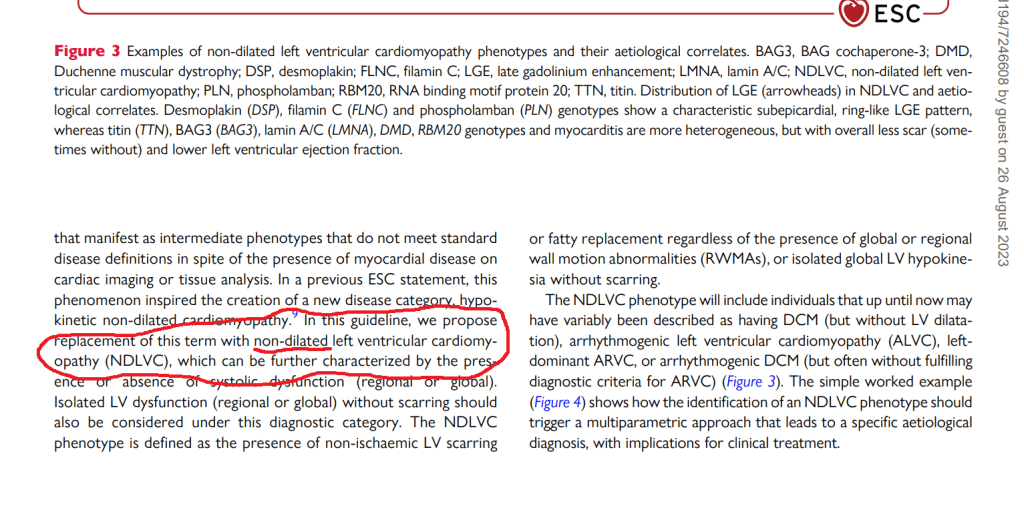
ESC, has come out with this new update on cardiomyopathy. It is a pleasant surprise to find the term “Non dilated cardiomyopathy” entered the cardiology academia, authenticated by the ESC.
I must confess, it is difficult to conceal the joy and a little bit of self-pride.
Some observations from this document
1. Despite our tremendous knowledge base, we are yet to hang up our boots, in pursuit of an Ideal cardiomyopathy definition. Genotypic or phenotypic ? Phenotype is closer to reality, while genotype is largely imaginary. It looks like, The newer guidelines are moving towards a phenotype-based approach in all aspects except in risk prediction. Fair enough.
2. All cardiomyopathies, whatever way we segregate, ultimately end up in the common clinical syndrome of heart failure. So. it is better to spend some quality time here and concentrate on HF therapeutics.
3. Cardiologists are expected to critically fine-tune their general medical knowledge, which will help recognize and treat systemic disorders like Amyloidosis, and other metabolic infiltrates.
4..Almost all RCMs have non-dilated ventricles, so why a new term NDLVC? Anyone wants to ask this question ?. Further, there can be significant overlap between RCM & NDLVC as well. Definitely, there is a lot to understand beyond this 2023 document.
5. Why do some ventricles refuse to dilate even in the face of adverse hemodynamic and pathological conditions. Is it an advantage or disadvantage? If ventricles are adamantly stiff and decide not to dilate, there is no other option, the atria will proxy dilate, creating more problems in the lung circuits. This also raises a fundamental question Is NDCM a better stress buster (think Laplace law ) than DCM? or vive versa , the accomodative nature of LV passify & blunt the slope of LVEDP at times of exertion.
6. One more reality is, NDLVC is also an Important subset in the now fashionable HF entity HFpEF
Final message
The message to youngsters is this. Discuss, debate, and document your thoughts in whatever forum, that is available. Don’t wait for all those big brother journals and their recognition. If there is truth in your writing, someday it will be revealed to the world.
Reference