Restrictive LV filling is an advanced form of diastolic dysfunction. The mean LA pressure is high, and LVEDP is also correspondingly elevated (need not be linear though, as LA reservoir/conduit dysfunction can independently hike the LA pressure). This clinical scenario of restrictive LV filling usually occurs as part of HFpEF, though it can occur in HFrEF as well. (25% of DCM have restrictive filling)
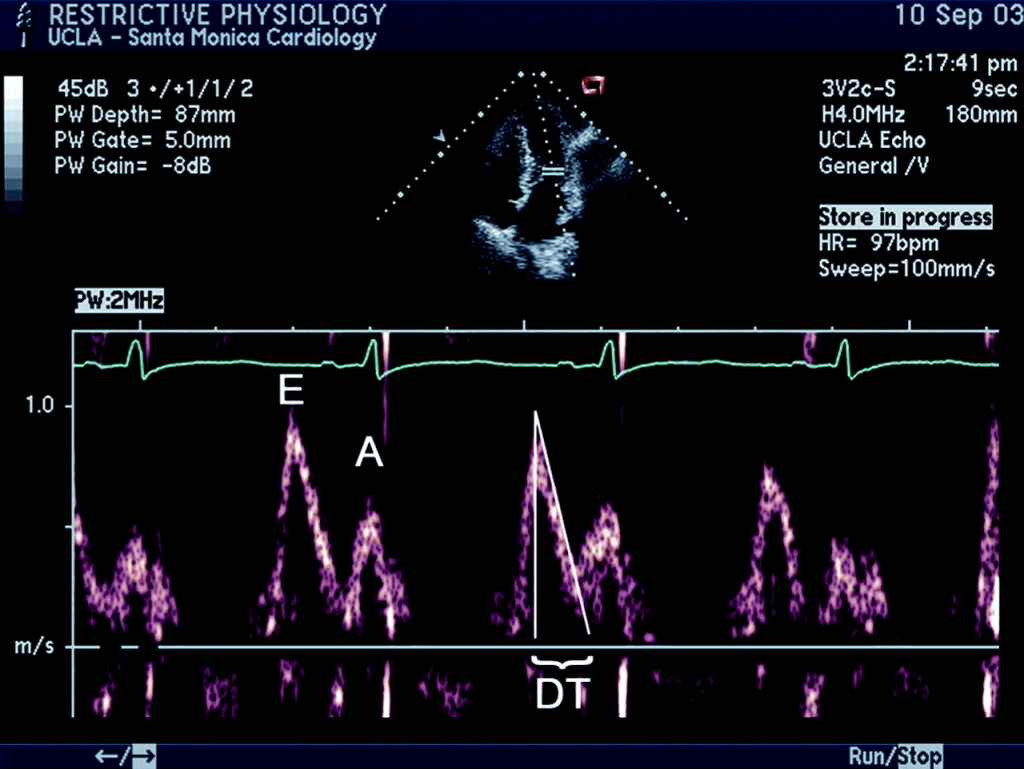
Image source and courtesey : Sean Haney, Denise Sur and Zijian Xu The Journal of the American Board of Family Practice May 2005, 18 (3) 189-198; DOI: https://doi.org/10.3122/jabfm.18.3.189
Pre-load reduction is the mainstay in relieving pulmonary congestion, but it has a trade-off at a particular point, as it impacts the stroke volume and forward cardiac output. Diuretic excess, ultimately worsens the symptoms, especially fatigue, though they keep the lungs dry.
So, dear fellows , remember prescription of diuretics in restrictive LV filling is a tight pharmacological rope walk.It requires continuous monitoring of symptoms and E/E” in echocardiography.
“Whether to push the LA blood with more preload or bring it down to redcue pulmonary congestion is the question“
Some physicians use the E-DT as a visual guide (Deceleration time of E velocity, which is inversely related to the degree of restriction). Normal is more than 150 ms. In most restrictive filling, it is 100 ms or less. Diuretic dose can be adjusted based on E-DT.
The usual daily dose of frusemide is 80 mg. There is a huge upper limit.It will be useful if the dose of frusemide is somehow indexed to the LV filling parameter.
I have tried a personal working formula for optimal diuretic dose. It can be titrated upwards ,twice the value of E-DT when it is less than 100 ms.(Eg if E-DT is 80ms Frusemide can be 160mg, but, note there is an U curve in this .If DT is too short, diuretics will worsen the hemodynamics .At 60 ms E-DT diuretics need to be reduced to 120 mg )
I keep tellling my fellows to do an authenticated study on this. Hope some one pursues(Mayo clinic guys are well equipped to do this , may be with the help Dr Jae.K OH or Sherif F Nagueh from Methodist, Houstan, the pioneers in the field )
Final message
We realise, treating restrictive LV filling is a delicate and often difficult task.There are no specific drugs to improve the lusiotropic property of LV. Further, since LV contractility is normal in HFpEF, there is no point in using LV inotropic agents. The only available parameter to manipulate is LV preload. However, It would be a stunning discovery , if some one discover a atria specific LA inotropic agent to overcome the LV restriction .
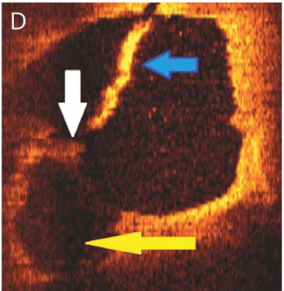
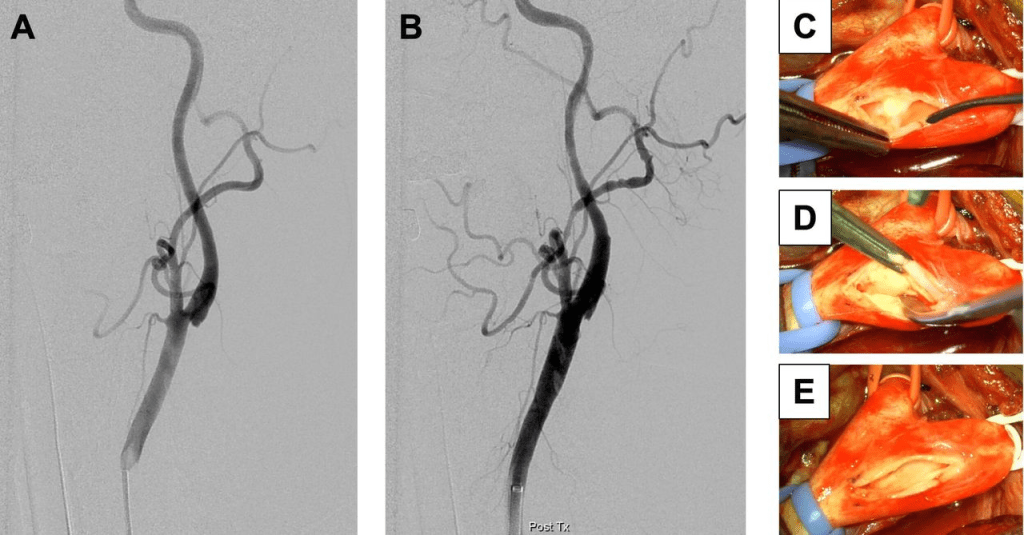
Meanwhile, it is critical to treat associated HT, CAD, or infiltrative disease like Amyloid*. We may soon have LA sensors , that can throw LAP to your iPhone . Till then, treating restrictive LV filling is essentially a hemodynamic/clinical pharmacological guess game. Ofcourse ,*We do have protein unfolders and declutters like Tafamidis & Patiseran to clear interstitial amyloidosis. Also, IAS flow regulators are new devices being tested to decompress the LA in HFpEF. (Paitazoglou et al Ther Adv Cardiovasc Dis. 2020 )