A 5-minute session: Answers are my own. Please cross-check.
1. Is Brugada syndrome clinical or ECG diagnosis?
Always clinical. Never get confused on this.
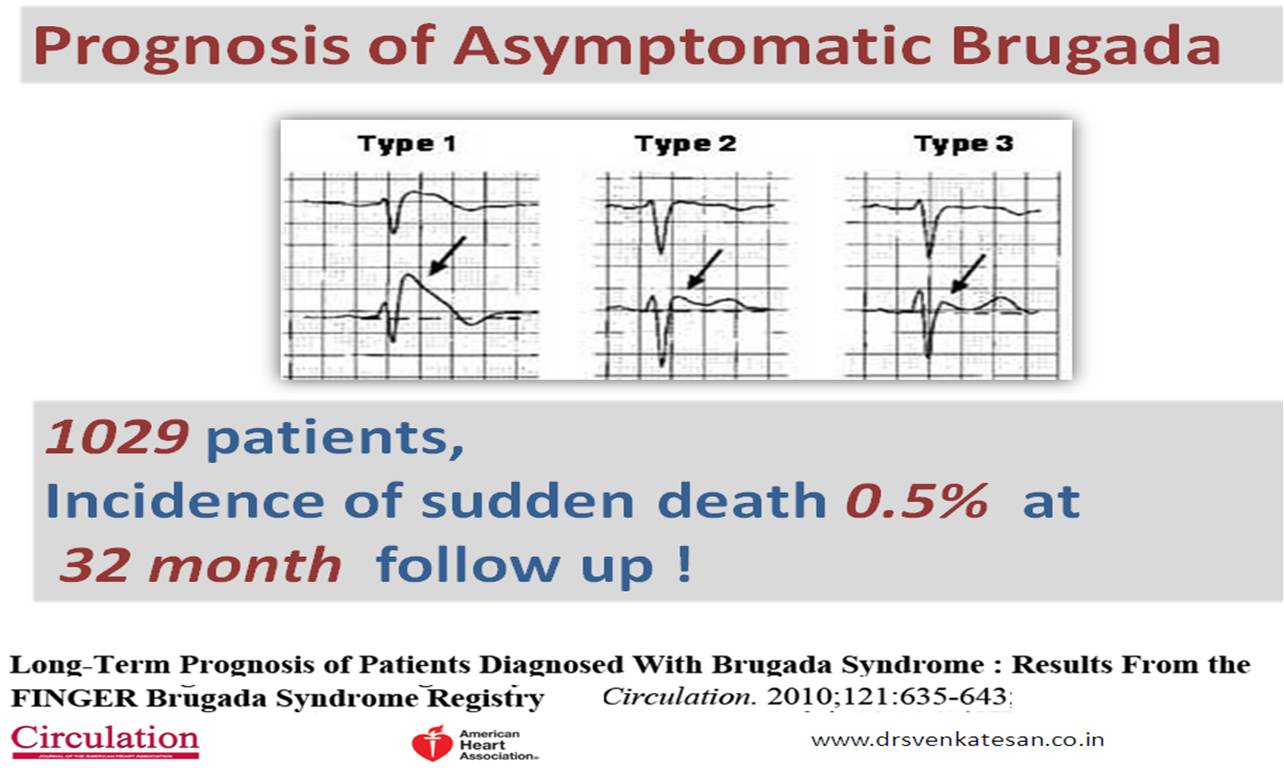
2. Spontaneous type 1 vs Induced Type 1 (from type 2) which carries more risk?
Both are risky since they are close cousins. But, spontaneous type 1 is the dreaded devil.
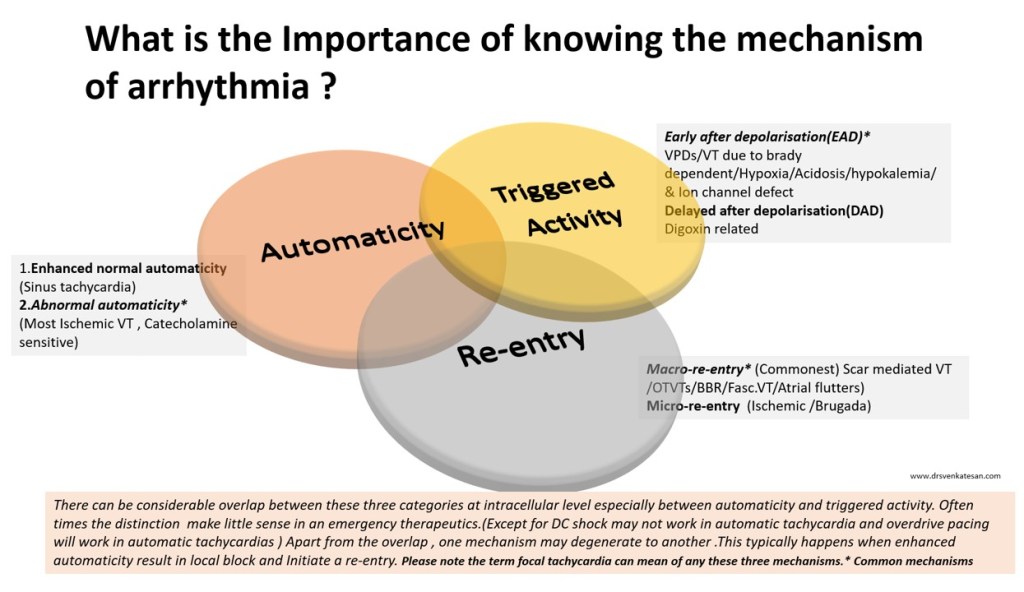
3. Is Brugada primarily a defect of myocardial depolarization or repolarisation?
Not clear. Often in both. In fact a mismatch between them. (Don’t ask how Na+ Channel defect affects repolarisation !)
4. Is Brugada VT is monomorphic, polymorphic?
Both. What determines morphology is not clear though. (All de-nova monomorphic VT will degenerate to polymorphic en route to cardiac arrest)
5. Should Fever induced Brugada pattern be investigated further?
Better, it is not to be reported in ECG. May not be important in the majority if there is no adverse family history. (If the patient is well educated and afflicted by Dr.Google and cardiologists can’t escape from ordering sophisticated tests)
6. What is the overlap between ERS and Brugada?
It is all about the Idiosyncrasy of the K+ channel phenotypes ( Transmural dispersion heterogeneity )
7. Is a benign Brugada better than a malignant ERS?
Yes, it would seem so. (Inferior or Infero -lateral ERS prone for primary VF in case they develop ischemic / ? also non-ischemic stress)
8. How important is the link between Brugada and Long QT 3 syndrome?
A rare entity, but It is double jeopardy for VT risk. The entire action potential width is vulnerable right from phase 0 to 3 or 4 A case report Sandhu A Clin Case Rep. 2017;5(8):1315-1319.
9. Is Amiodarone really contraindicated in VT?
Not really. Though Amiodarone unmasks Brugada, it can still be used during episodes of VT in patients with manifest or unmanifest Brugada. Maybe in Long QT 3 overlap, it may perpetuate the VT.
10. How important is the structural myocardial defect in Brugada?
Not important in the majority. Though localized RVOT abnormalities are noted in some..RV abaltion can be succesful in odd case.
11. What happens to the ST segment in Brugada during exercise stress?
ST-segment may normalize in some. A stress test can help to risk stratify. Subramanian M, J Cardiovasc Electrophysiol. 2017 Jun;28(6):677-683.0
12. Which drug is probably best for Brugada as of now?
Quininde , A fairly specific blocker of Ito current. However, it needs to be used diligently. Management of Brugada Syndrome: Belhassen B, Rahkovich M, Michowitz Y, Glick A, Viskin S Circ Arrhythm Electrophysiol. 2015 Dec; 8(6):1393-402.
13. Is ICD definitive therapy?
Obviously not. But, definitely life-saving in high-risk survivors. I guess definitive therapy is possible for future generations through the science of genetic reprogramming of Na+ channels. (Of course, our planet shouldn’t succumb to man-made climatic arrhythmia, by then )
14. Does widespread genetic testing & screening of families help in the management and reduce anxiety?
Cracking the genomic code of cardiac ion channels is the ultimate sophistication (Blueprint of fate ?) However, there is no guarantee this information is going to ease out the family members who harbor a genocopy with or without a phenocopy.
15. Is Brugada getting undue attention in cardiology literature compared to many other common arrhythmias?
You can answer this …………………………………….
Further reading