I used to tell my students ,the relationship between the heart and kidney is so close , it is never justified for the two departments of Nephrology and Cardiology are physically away by two blocks in our institute .
Kidneys are vital to maintain the volume and pressure of body fluids and heart is responsible for keeping this fluid circulating.
In clinical setting it is a well known secret ,most deaths in patients who are on dialysis is cardiac while most deaths in patients with CHF are renal.
It remains a mystery why kidneys were ever considered as a circulatory organ , when our medical pundits de-compartmentalised human organ systems !
CKD is pre-cardiac failure and CHF is pre-renal failure
The Heart /Kidney affair is so intimate in many pathological situations both either succeed or fail simultaneous or sequentially.
While CKD results in and pressure and volume overload of heart , cardiac failure cause pressure and volume under load (pre-renal factor) which worsen the renal function and aggravate cardiac function alter.
In essence, it is vicious cycle of two serial organs performing the vital circulatory function with body fluids playing a role of diligent mediator.Whenever the kidney fails heart is stretched and stressed to its Frank starling limits by the volume as well as the accompanying HT load.
While text books link these two organ as simple cardio-renal syndrome it is not happening at the level of patient’s bed side.
Cardiologists and Nephrologists must realise they need do work in tandem like their respective departmental organs which accomplish this task easily !
To tackle this much maligned cardio-renal conundrum
Consider CKD as CHF equivalent and CHF as CKD’s
I would recommend this concept to be infused right in the third year medical school and try de- compartmentelise clinical medicine.
Need of the hour : How to Moderate ACEI dosing in CKD
ACEI has been a major pharmacological revolution in controlling and reversing the adverse events of cardiac failure . Some where along , a significant fear complex arose regarding the damage it could cause to kidneys.
Recently , we know the role of ACEI in CKD made U turn(Like what Beta blockers did to CHF) .Now, it is presumed ACEI are indeed safe in most CKD and may even regress CKD. Still this concept has not been fully disseminated into general physician domain.
Let cardiologist and Nephrologist sit together and sort out this issue.
I guess , ACEI controversy is a sort of ongoing ego clash between Nephrologist and Cardiologist . Both like it , both make fuss about it ! In my observation , if a cardiologist titrate it upwards Nephrologist would lower it and reverse happens if cardiologist express caution about it ! Do you agree ?
Final message
Mankind has accrued great benefits from stunning break throughs in modern medical science . . . but it has come only at a huge cost ! Medical knowledge has completely fragmented the physician mind-set .Every good therapeutic concept is hanging aloof .It requires periodic de-fragmentation (As we do it to our PCs by anti-viral soft ware !)
To begin with , let us consider CKD and CHF as single sequential circulatory entity !
Let us vouch to create new generation medical professional devoid of skewed medical vision !
Reference
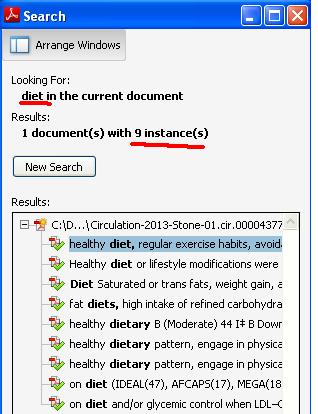
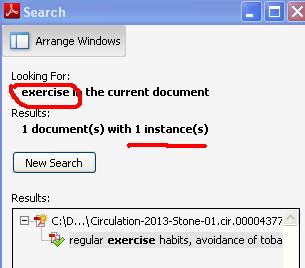
Guidelines for ACEI in CKD

https://www.kidney.org/professionals/kdoqi/guidelines_bp/guide_11.htm
Read Full Post »