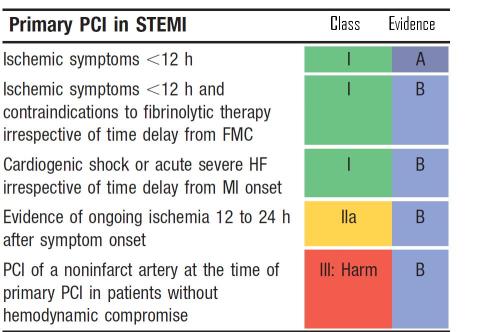
Primary PCI is presumed to be the ultimate , undisputed reperfusion strategy in STEMI . Still , time and again one study or other strips down this “Numero Uno” status of pPCI . If it is really supreme , such awkward situation shouldn’t arise too often . More importantly , the major reason for dubious real world record of pPCI goes beyond the time and logistic factors (which is considered the only issue for pPCI by most interventionist ! ) There is something more to it that is invisible ! (Is it the no reflow ?)
The nearly flawless study from Belgium ( STREAM Just released in ACC 2013/Sanfransisco ) , pre-hopsital or early fibrinolysis has proven to be superior in the prevention major end points at 30 days .
- Death
- Re-infarction
- CHF
The major surprise was pre-hospital fibrinolysis showed less incidence of cardiogenic shock . ( pPCI
group had more of this ( 4.4 VS 5.9 % in STREAM )
Now . . . shall I make a provocative statement ?
while pPCI may be treatment of choice for cardiogenic shock . . . but it may also confer a risk of cardiogenic shock in otherwise low risk MI !
Caution and conclusion
STREAM population applies strictly to 1 to 3 hour time window . It does not apply to either before or after that ! Simply put,we do not have guts to compare fibrinolysis and pPCI in patients who arrive within one hour into a facility where 24 hour cath lab facility is available . We call it unethical to do a study like that ! I personally feel it is really unethical if we do not do a study in this time frame . The reasoning is simple and very personal .In a large Government hospital where we do not have primary PCI program our net mortality for STEMI never exceeded 7-8 % over a period of 10 years , Which is almost at par with global data on pPCI. (Our door to needle time is an unbelivebale 8-12 minutes ! that too only streptokinase !)
Adding Further controversy
pPCI is indeed a superior reperfusion strategy . No one can dispute that .But its superiority is not realised in every patient who gets it. The benefits are accrued if and only if it is used most judiciously . In Low risk , small regional , branch vessel STEMI , pPCI has never been shown superior . It is well recognised , upto 15 % of STEMI is likely to spontaneously abort or experience very good spontaneous recannalisation . By rushing these patients very early into cath lab pPCI meddles with the natural anti fibrinolytic mechanisms . It is this population who invite all the procedural hazards. .
Is this the reason STREAM had more cardiogenic shocks in pPCI limb ?
I think STREAM has strengthened the case in favor of fibrinolysis in this ever ending debate .
I would seriously believe pPCI is hanging it’s superiority over fibrinolysis with a wafer thin mortality advantage . pPCI may not be recommended in a routine fashion to all STEMI population even if they arrive within 6 hours and able to perform the plasty fast . Science is . . . after all . . . continuing confrontations with our assumptions !
Counter point
STREAM is not an exclusive study comparing fibrinolysis and PCI . It is a study comparing Pharmaco Invasive approach vs pure invasive approach . 80 % of patients in the fibrinolytic limb ultimately received PCI and stenting . It simply doesnot make sense to conclude fibrinolysis is superior to PCI . Most of the beneficial effects on 30 day outcome may reflect the timely PCI in the lytic group.
//