Some physics: Why is blood under pressure?
In perfect vascular climatic conditions, the human circulatory system is comparable to a smooth flowing river irrigating 100 trillion cells, traversing many kilometers of the capillary network, to the far away tissue bed. One major difference in the river analogy is, that in human biology, the entire blood has to return back to the heart in about 30 seconds. (The fact that the venous system does this in style with near-zero pressure head is the greatest wonder in circulatory physiology)
The force per unit area, that drives the blood is the blood pressure. It is expressed in kilo pascals. (16/10 Kpa one Kpa is 7.5 mmHg. It has two components streaming pressure as well the lateral pressure. What we measure by conventional BP apparatus is the lateral pressure on the vessel, which is what we are worried about most times. But, the forward driving head is equally important because the branch points bear the brunt of this pressure head. Sudden surges and spikes attack the grade separators more. This is one of the reasons, the arterial branch points are more prone to atherosclerosis. Though we believe onward pressure head does all the damage, it is also worth knowing the velocity of blood flow can also be defining factor in vascular Injury. The flow velocity is surprisingly low in physiological conditions, about 4-6km/h something similar to our walking speed.
What is normal blood pressure?
We don’t know. The search is going on. But, what is important is the net lifetime BP harming effect on blood vessels. Of course, BP is not a mono player, it interacts with other risk factors like lipids, diabetes, and smoking, along with genetic susceptibility, and epigenetic vulnerability, making cardiovascular events perfectly polygenic.
How do we define and grade systemic HT?
A dozen different societies keep defining this (ACC/AHA. ESC, ISH, British, whatever be the normal, one set of numbers is permanently etched in our mind ie 120/80 as the cut-off.
A more philosophical definition would be, that high BP is defined as the BP at which our blood vessels feel the stress and strain and begin to wear out. We may never ever know that in a given patient. Now, we are adding more twists to this already confusing normality data. Namely nocturnal BP.
Why 24 hr /Nocturnal BP important?
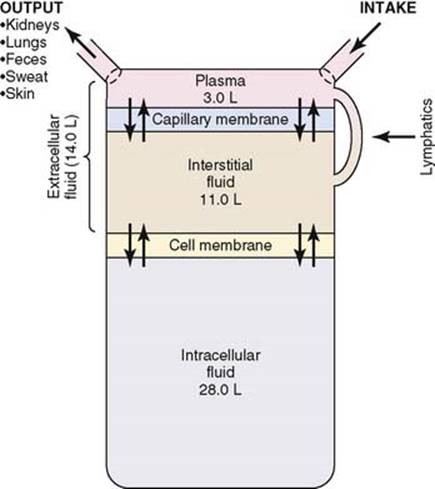
If the average human lived for 75 years, he or she will be spending 25 years in sleep. What does our circulatory system do in those 25 years? We don’t know. We believe if the brain sleeps the vascular tree takes rest as well. How can it be? The reticular activating system should go off mode, still the vasomotor centers should be vigilant enough to keep vital organ perfusion. Ironically, sleep can be stressful for some. During recumbent posture the fluid compartment redistributes and ECF expands especially in patients with renal and cardiac compromise. (Recall the mechanism of PND) .Add on to this, the ever-fluctuating sympathetic tone with REM/NREM sleep phases. One of the offshoots of widespread use of ambulatory BP monitoring is (ABPM)is the new term nocturnal hypertension.
Defintion of nocturnal HT
The definition of nocturnal hypertension is, night-time BP ≥120/70 mm Hg (Now it is more stringently defined as >110/65 mm Hg by the 2017ACC/AHA guidelines. I am not sure, but I think this is applicable to anyone with or without HT irrespective of treatment.
Two more entities exist to confuse us. Just don’t bother. (Fellows can’t escape from this though). A Clinic and morning home BP of <130/80 mm Hg is defined either as masked nocturnal hypertension or masked uncontrolled nocturnal hypertension if they are already on drugs.
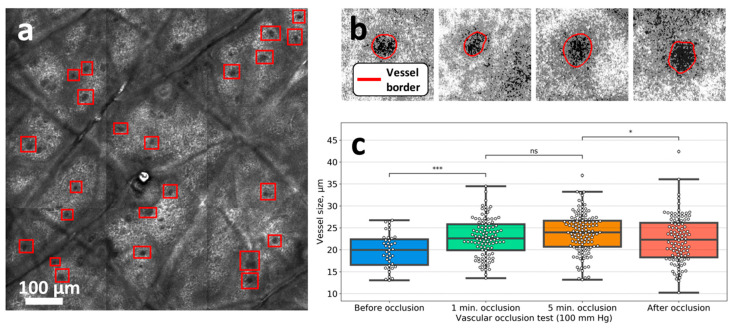
Night time BP patterns
Normally we expect 10 -20% dip in BP is expected.
The following are four nocturnal BP patterns defined:
- Dipper: 10-20 %;
- Extreme dipper, more than 20%;
- Non-dipper: less than 10%,
- Riser: 0%.or + side (I think, this is the same as the reverse dipper )

An Important resource from HOPE Asia net work on ABPM Kazuomi Kario Journal of clinical hypertension.https://doi.org/10.1111/jch.13652 While everything looks ok, that blue line amuses us the most. These guys are also called reverse dippers.
Nocturnal dipping: Is it systolic, diastolic, both or mean?
Most studies documented as systolic dippers. Dipping is expected to Impact both systolic and diastolic BP similarly. But, we know it need not be. systolic BP is more volume-dependent, while diastolic BP is resistance is related. I think the concept of diastolic vs systolic non-dipper is yet to be evaluated.
How to measure? How many readings?
- Ambulatory BP monitoring equipment is the key. Few companies have defined and have patented software (Omran HEM series is the leader, Micro life is another one )
- The night-time BP is calculated as the average of night-time BPs (from going to bed to arising) measured by ABPM The number of night-times BP measurements required may be ≥6.
- The methodology is getting standardized. Errors in measurement are considerable. Posture, temperature, and inflation triggered awakening all matters.
-
Substantial technology is still evolving. Remote wireless monitoring is possible (Apple and Google are keenly watching the global BP market potential !)
Management issues
Though there are 4 subsets in nocturnal BP patterns, currently, Identifying non-dippers is the key target that will help diagnose more resistant HT.
How to convert non-dippers into dippers?
- Night-time dose of antihypertensive drugs to be encouraged.
- Salt restriction in the evening diet
How to prevent excessive dipper (>20%)
The reverse of the above advice is true in this subset.
Isolated nocturnal hypertension
I think it is an overzealous concept in sleep medicine. Let us wait and observe. Stojanovic, M., Deljanin-Ilic, M., Ilic, S. et al. Isolated nocturnal hypertension: an unsolved problem—when to start treatment and how low should we go?. J Hum Hypertens 34, 739–740 (2020).
Is there a J curve phenomenon among dippers ?
We cant generalize, pro-dipping forces are good & non-dipping forces are bad. Should we consider labeling excessive dippers as nocturnal hypotension? Considering the fact both non-dippers and excessive dippers carry more CVD risk. Like any other biological variables with dynamic safety margins, we are clueless about what is ideal dipping .(A nocturnal J curve)
Clinical trials on nocturnal hypertension
- JHOP study Kario K, Hoshide S, J Clin Hypertens 2015 from Japan is a very popular one on this topic.
- While this elegantly done Finish study (J.Hypertension 2004 ) stressed the importance of home BP monitoring.
What is new in nocturnal HT management?
Melatonin, administered as circadian hormone therapy is expected to play a useful role as a night watchman in BP control (Frank et al Hypertension 2004)
Final message
Nocturnal hypertension is trying to emerge as a new cardiovascular risk factor. Understanding this condition and intervening seems to be important, considering the well-known fact, that cardiovascular events are clustered in the early morning hours.
Still, routine ABPM to know the status of nighttime BP in all hypertensive individuals is not warranted. However, people who had an event or who have secondary hypertension may need to do so. The simple truth is if you have a peaceful day and a perfect sleep, your BP is bound to dip naturally. So, the message to all those active and energetic men and women who are carrying a tag of hypertension need not worry about this dipping and non-dipping stuff. Instead, maintain a healthy lifestyle. There is a thin line separating awareness and anxiety.
Reference
1.Yano, Y., Kario, K. Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertens Res 35, 695–701 (2012). https://doi.org/10.1038/hr.2012.26
2,Cuspidi, C, Sala, C, Tadic, M, et al. Clinical and prognostic significance of a reverse dipping pattern on ambulatory monitoring: An updated review. J Clin Hypertens. 2017; 19: 713– 721. https://doi.org/10.1111/jch.13023