Reviewing NOTION study, the Nordic TAVI 10 year follow up has just been released (Ref 1) :
Caution :Non-academic content
This study reports the long-term outcome in low-risk individuals who required AVR. The study basically compared the blind and passive deployment of bio-prosthetic aortic valve aided by the catheter skills of new-age cardiologists with sophisticated image backup versus Open surgical replacement of the aortic valve by experienced cardiac surgeons, after meticulously removing and debriding the native leaflets and suturing the prosthetic valve permanently in the optimal target site under direct vision.
Study summary
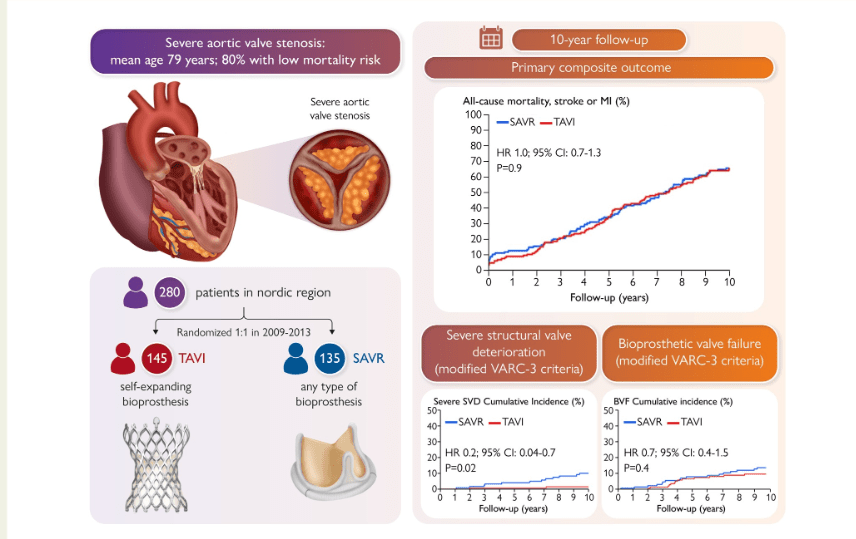
Conclusion
The study results finds the valve deployed percutaneously under semi- blind vision, was equipoise with SAVR done under direct vision. The surprise however is, TAVI was superior to cardiac surgeons in multiple aspects .The mysterious finding is TAVI had less Structural valve dysfunction, and possibly low bio valvular failure (BVF), if Kaplan -Myer curve trend is little extrapolated. No doubt ,the Aortic interventional world is applauding and everyone is joining the party.
Now, some academic queries ?
1.Did the trial compared best practices of TAVI & SAVR ?
No. Because it was done in 2010-2013. (Which grew faster TAVI or SAVR in the last10 years ? in terms of both hardware and expertise . How it will impact now ?)
2..Was the outcome assessment blinded ?
No
3.Why there is 50 % cardio vascular and 60% all cause mortality in both groups even though they belong to low risk category ?
Don’t know. Not clear.
4.Why the gradient was high in SAVR in the follow up ?
There are two important factors. More than 98% of TAVI patients had a valve sized 26–31 mm, while 98% of SAVR patients received a size 19–25 mm . Apart from valve size aortic annular enlargement before SAVR was not done in majority, there by enhancing the gradient and valve mis-match.(Note :The TAVI begins at 26mm and SAVR ends at 25mm. For how many of you this looks odd ?)
4a. Was doppler velocity index measured in all to assess EOA in follow up ?
No. It was not mandatory.
5..Is it Ok to define structural valve dysfunction(SVD) based on gradient alone ? Did TEE/CT follow up imaging done ?
No. Flow is physiology. Sub physiological valve destruction very much possible without affecting gradient.
6.The rate of severe SVD was higher after SAVR. Is there any meaningful explanation why surgeons valve deteriorated fast ?
No .
7.Was CAD accounted for outcome difference ?
No .CAD patients were excluded.
8.Did this study address technical issues in performing PCI with new onset CAD and its possible impact in outcome
No. TAVI induced coronary ostial encroachment not reported.
9.Why didn’t they use bi-leaflet mechanical valves in SAVR group ?
Don’t know .(*One possible reason is given in the foot notes)
10.Is this study still valid ?
Sorry, I don’t know.
Final message
Whatever is written here, NOTION will remain a great study with a 10 year meticulous follow up . As a cardiologist, very soon we will be allowed legally to choose TAVI even in more younger , low risk cohort of Aortic stenosis without co-morbid conditions. Still, if you put patient first approach ,CAUTION should precede NOTION .
* One version of answer for question 9 , would be TAVI vs Bi-leaflet St-Judes study was in-fact proposed, but was apparently not approved for (un)ethical reasons, of comparing a short living bio-valve valve with a long lasting mechanical valve.
Reference
1.Hans Gustav Hørsted Thyregod, Troels Højsgaard Jørgensen, Nikolaj Ihlemann, Daniel Andreas Steinbrüchel, Henrik Nissen, Bo Juel Kjeldsen, Petur Petursson, Ole De Backer, Peter Skov Olsen, Lars Søndergaard, Transcatheter or surgical aortic valve implantation: 10-year outcomes of the NOTION trial, European Heart Journal, 2024;, ehae043, https://doi.org/10.1093/eurheartj/ehae043