Coronary bloodflow is primarily known, to occcur as a diastolic circulation. Does that in any way mean coronary artery diastolic pressure, can exceed the systolic pressure ?
A. No. diastolic BP can never exceed systolic BP in side the coronary artery.
B. Yes. Coronary diastolic BP is higher than systolic, since there is little blood flow during systole due to myocardial compression.
C. There is not much difference between systolic and diastolic pressures, within the coronary artery . We need to bother only about mean perfusion pressure.
D.It is true, the coronary blood flow is compromised in systole and primarily occur in diastole .Still, the epicardial coronary arterial compresssion is not that significant. Hence systolic pressure blunting is negligible. This is called the pressure -flow paradox.
Answer : D (Ref Image 2)
What is the normal intra-coronary arterial pressure in systole and diastole? I could not get a clear answer to this question. Logically it should be sane as in radialartery 120/80mmhg. Surprisingly, most literature discusses only coronary blood flow, which primarily takes place in diastole. (Does that mean the pressure would be less in diastole, so that blood flows easily?) The complexity in understanding intra-coronary pressure , is because, we don’t know the exact blood volume, flow vs pressure relation in this dynamic organ.Further, mechanical force/pressure exerted by the muscle ,can it be recorded , within the lumen , and quntify it sepearately ?
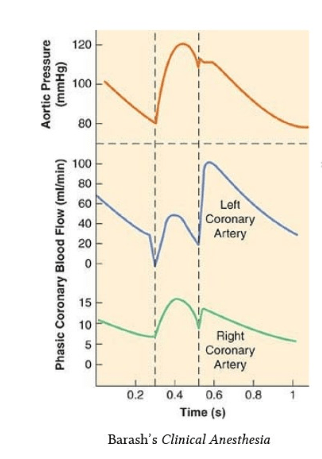
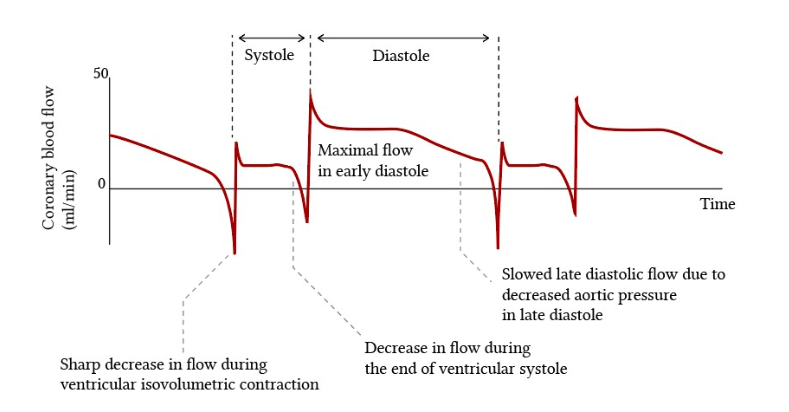
The classical illustrations that are found in cardiac physiology literature about the dominance of coronary blood flow during diastole (Image source Ref 2)
During FFR studies the Intracoronary presssure curves almost mimic radial pulse. No where we could see the effect of mechanical compression . It is likely , the epicardial coronary artery do not get compressed that much , only the micro circulation gets squeezed.
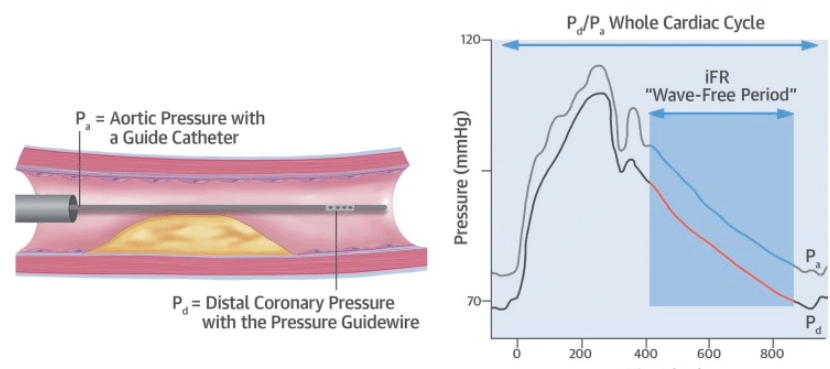
Image 2: source Yuhei Kobayashi et al JACC 2017
We realise ,coronary perfusion pressure, mean coronary arterial pressure, and coronary arterial wedge pressure are more important than systolic and diastolic pressures . The mean coronary artery pressure is around 45 to 60 mmHg backed up with good autoregulatory mechanism. We are not clear how this autoregulation is modified by lesion tightness. Documentation of true coronary arterial systolic BP in physiology and various pathologies is an important academic vacuum that youngsters can explore.
1.Clinical Implication : Does LV dysfunction has a favorable efffect on coronary perfusion ?
If LV contraction interferes with coronary blood flow, patients with severe LV dysfunction, may gain some advantage as systolic blood flow can happen more easily, and myocardium is perfused better, provided the aortic systolic pressure not too low enough.
2.How common is angina in DCM ? and Why ?
Angina in DCM is an exception despite elevated LVEDP. Is the above logic explain why very few dilated cardiomyopathy patients experience angina? Even in ischemic cardiomyopathy, once it sets in, Intensity of angina is mitigated or completley eliminated.(of course at the cost of failure). Is it nature’s response to prevent angina?
3.Why systemic hypertension is a weak coronary risk factor ?
Unlike the brain, where stroke risk is directly related to systolic BP, fortunately sudden systolic spikes rarely get a chance to attack the coronary endothelium as much of the coronary lumen is relatively closed (? to be confirmed , atleast during rapid ejection phase of systole) In this context, we can also be happy there is no risk of myocardial hemorrhage due to HT. However, there is evidence that diastolic BP carries much risk for CAD, as do Isometric exercises when DBP exceeds out of proportion to systolic BP.
4.Differential intra coronary pressure , RCA VS LCA is well knwon asthe RV contraction is not good enough to compress the RCA.This adds a new hemodynamic concepts in RCA CAD.(We have done a study where we found thrombolysis was more effective in RCA apparently due to bi-modal continuous delivery of the lytic drugs, unlike the left system)
5.During CPR , what would be coronary hemodynamics of chest compression ?
When we compress, it is systemic systole, and when we release it becomes coronary diastole. In fact there is now evidence to suggest , too rapid and hurried contractions reduce the success rate of CPR. The inter compression time is to be atleast 4 or even 5 full seconds, to enable coronary perfusion.The mean pressure during CPR is to be atleast 40mmhg. (Yannopoulos D et al , Resuscitation. 2005)
Final message
It is surprising why we are not recording intra-coronary pressure directly and trying to understand this. We need to go 100 years back for that Wiggers article in search of truth. (Ref 1). This is an area of good research for cardiology fellows. Also, next time,when you do FFR or IFR, ask this question : Why proximal reference pressure is taken at the aortic root instead of just before the lesion ?
Reference
 A normally functioning circulatory system is vital for our survival . We have about 6000 ml of blood, circulating all over the body in an approximate time of 15-20 seconds.The pressure at which this blood moves across the body is called the blood pressure . Hypertension or simply , high blood pressure is an undesirable hemodynamic disturbance in human circulatory system.Systemic hypertension is the most common type of hypertension. The blood pressure is primarily dependent on the status of the blood vessel(vascular resistance) and cardiac contractility. This regulation is under many neural and hormonal factors.Further the blood pressure varies depending upon the blood vessel calibre, and the local milieu.There is a progressive drop in blood pressure from major arteries to the small arteries .The pressure drop is maximum across the arterioles to reach the venules .The venous circulation has the lowest pressure, it ends up at right atrium with a mean pressure of 0- 5mmhg.
A normally functioning circulatory system is vital for our survival . We have about 6000 ml of blood, circulating all over the body in an approximate time of 15-20 seconds.The pressure at which this blood moves across the body is called the blood pressure . Hypertension or simply , high blood pressure is an undesirable hemodynamic disturbance in human circulatory system.Systemic hypertension is the most common type of hypertension. The blood pressure is primarily dependent on the status of the blood vessel(vascular resistance) and cardiac contractility. This regulation is under many neural and hormonal factors.Further the blood pressure varies depending upon the blood vessel calibre, and the local milieu.There is a progressive drop in blood pressure from major arteries to the small arteries .The pressure drop is maximum across the arterioles to reach the venules .The venous circulation has the lowest pressure, it ends up at right atrium with a mean pressure of 0- 5mmhg.

