LIMA to LAD anastomotic site lesion ,is an important subset of CAD that can occur either as acute post operative event or an ACS , CCS. Interventional cardiologists have, thus far, been reluctant to intervene in this type of lesion, often refer to a surgeon instead.
Here is case report by by Tahir et al. wherein a 75‑year‑old post‑CABG patient who developed acute LIMA→LAD anastomotic failure under cardiogenic shock within 24 hours of surgery. Considering the risk of of perforation or avulsion with standard PCI, the team deployed a PK Papyrus covered stent directly across the anastomosis—restoring TIMI‑III flow and myocardial blush successfully.
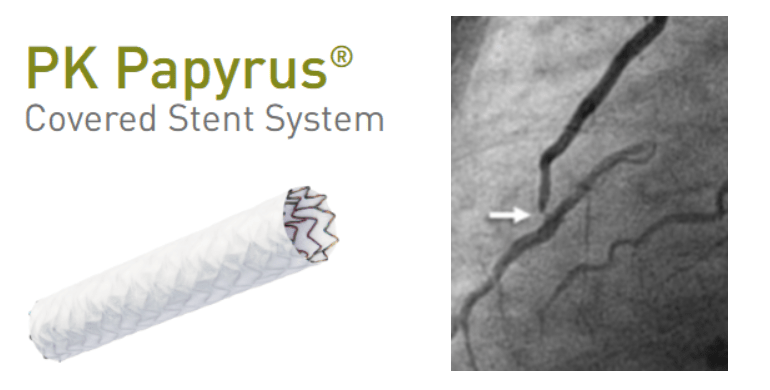
This highlights the covered‑stent’s potential as a first‑line semi‑emergency intervention, offering controlled sealing and avoiding repeat surgery in hemodynamically unstable patients.
What about chronic anastomotic site Lesions ?
Beyond acute rescue, the covered‑stent may play a valuable role in chronic anastomotic stenoses at the LIMA–LAD junction—lesions notorious for tortuosity and perforation risk. The PK Papyrus platform, with improved deliverability compared to older models like Graftmaster, offers a safer option for such high‑risk anatomical sites . Surprisingly, this indication is absent from covered‑stent guidelines, despite its clear utility in both acute and chronic settings.
Implications of blocking Native LAD Flow
There can be downsides in blocking the native LAD flow by the covered stent. ,However, in reality the proximal flow and to potential branches till the covered stent block is found to be flowing well. In contrary, a key advantage of covering the LIMA–LAD anastomosis is the elimination of competitive flow. In many bypass scenarios, flows between the graft and native vessel compete, potentially compromising graft patency. With the covered‑stent sealing the anastomosis, distal LAD circulation becomes exclusively graft‑dependent, which may actually
- Stabilize hemodynamics by directing full perfusion through the graft.
- Reduce competitive flow dynamics, promoting long‑term graft patency.
- Lower ischemic risk if native LAD disease progresses proximally.
- Finally, the cover acts as a distal protection device against thromboembolic material from proximal friable lesions.
Role of DEB /DES in LIMA to LAD anastomotic lesion
This can be an alternate option. If native LAD flow is considered important and lesion is less complex and risk of perforation is low.

Final message
A simple DOBA (Drug eluting POBA) , or a covered‑stent at LIMA–LAD anastomoses can be a game‑changer, saving lives in emergencies, possibly improving chronic graft outcomes as well. It’s time for interventional cardiology experts to recognize and acknowledge this application, supported by further registry data or trial.
Reference