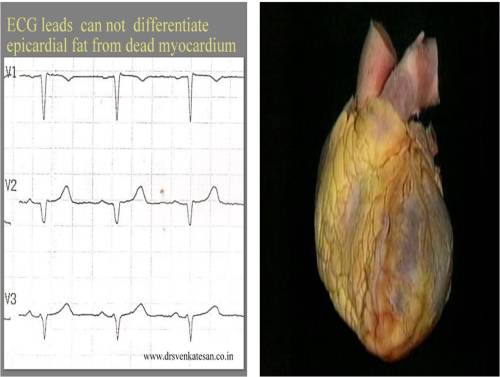
Surprises are hall-marks of medical science . The cardiologists do get it , in enough doses from echo labs on a regular basis ! . One such thing is the total ECG-ECHO myocardial territorial mismatch following a STEMI . Human myocardial segments are divided by cardiologists by 17 segments by echocardiogram . Long before echo came into vogue , electro-cardiologists divided the heart electrically into three zones to localise MI . (Anterior , inferior and the poorly defined entity lateral walls* ) .Inferior and posterior segments are almost used interchangeably. So , when we have 17 echo segments to be fit into these three electrical category ! were bound to have some overlap . The issues of fitting in septal segments is really complex as septum is a three dimensionally engulfs all three electrical surface of the heart .
* By the way , anatomists never agreed about existence of walls in heart.They simply said , heart has smooth surfaces that blends with one another. We cardiologist have built imaginary walls and struggling to come out it !
We will try to answer the question that’s been asked here . “Inferior MI” by ECG . . . “Anterior MI” by echocardiography . How common is that ?
Possible causes for this wrong call
Technical errors in acquiring echo imaging plane or it’s interpretation is the commonest . Many times , obliquely obtained long axis view wrongly and strongly suggests a septal MI instead of inferior posterior MI. This is because in apical 4 chamber view bulk of septum (Basal and mid third ) lies in the infero-posterior region .

Perhaps , misunderstanding this septal geography is the commonest cause for erroneously calling inferior MI as anterior in echocardiography . (A simple clue is the presence of MR . (It fixes the infarct in infero-posterior zone with 90% accuracy )
Rotation and posture of heart
Alignment of the septum to the rest of the chambers can influence , how three inferior leads is going to look at the septum (There can be considerable errors -Electrical myopia ? as these leads are located distantly ) . The plane of the septum is such that in horizontal hearts septal electrical activity will be directed infero posteriorly inscribing a q waves in inferior leads rather than anterior leads . One can expect such ECG /Echo discrepancy in the following subset as well
- Post CABG patients (Any pericardiotomy will make the septal motion erratic )
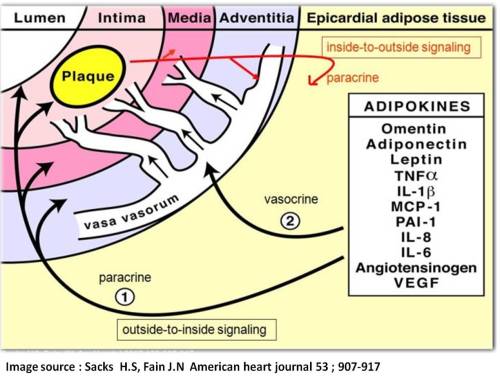
- Obese persons
- COPD
There are three more situations , which mystified me with definite ECG/ECHO mismatch
- LVH and STEMI is always an engima . Counter clockwise rotation when accopany LVH that masks anterior MI electrically . It however inscribes a q wave in inferior leads.
- In dominant LCX lesions ( with at-least one major OM ) and left main bifurcation STEMIs , combination of anterior and inferior wall motion defects are quiet common . When a such a MI evolves ( with or without revascularization ) regeneration of R wave can be time shifted . Septal R wave may appear much earlier and inferior R may follow or vice versa . .Further, anterior MI may evolve as Non q MI making it ECG blind , still echo may pick up the WMA . So there can be important ECG-ECHO mismatch in myocardial segmental geography .
- Further , WMA need not always be an infarct .Any new episode of ischemia can result in WMA . Hence a patient with inferior Q waves in ECG may experience anterior wall motion defect meagerly due to fresh episode of ischemia (This we should not attribute to old anterior MI. It is also possible intra-myocardial conduction delays can elicit remote wall motion defects.
Final message
By general rule , ECG correlates well with ECHO for localising myocardial segments . At times , it can really be tricky , and we get into above situation in echo labs.
While , it is common to observe ECGs to mimic inferior MI at the first look and subsequently echo revealing anterior infarct , the reverse is also very much possible .
The mechanisms are varied and technical issues are for more frequent than true clinical discrepancy .The issue has important management implications.
Of course , coronary angiogram will pin point the anatomy , still it also has strong limitations in localizing myocardial segments (to which it supplies ) especially with multi-vessel CAD and collateral dependent circulation .
Read Full Post »