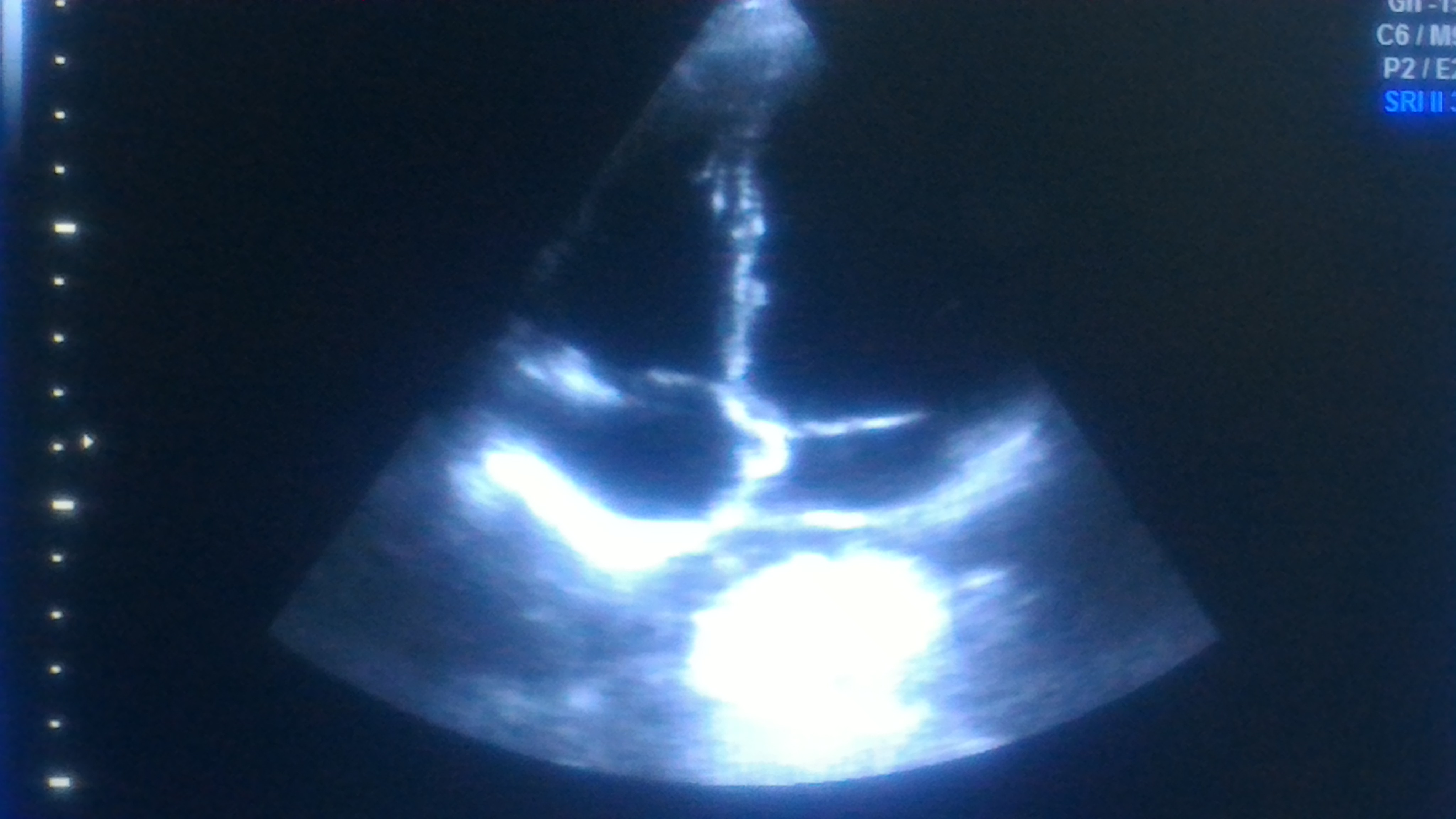
It is rare case and real tough one. A clue : concentrate inside the pericardial space. (36, year old man , asymptomatic)
Know the diagnosis
Source and reference & Courtesy
Comment : Most curious , who stopped it from entering LV ?
Posted in Uncategorized, tagged bullet injuries of heart, echocardiography, gun shot injury of heart, miracles in clinical cardiology, pericardial disease, rare cases in cardiology, rare foreign body in heart on January 27, 2026|
It is rare case and real tough one. A clue : concentrate inside the pericardial space. (36, year old man , asymptomatic)
Know the diagnosis
Source and reference & Courtesy
Comment : Most curious , who stopped it from entering LV ?
Posted in Uncategorized, tagged 1.5 vs 1 square cm, acc esc valvular disease guidelines, color dopler, dobutamine stress in mitral stenosis, echocardiography, excercise stress teting in mitral stenosis, jase, liv hatle, mitral stenosis, mitral valve orifice, moderate vs severe mitral stenosis, mvo, mvo by planimetery vs pressure half time, pressure half time, tran mitral gradient in mitral stenosis on November 26, 2024|
Right from the days we entered medical schools, severe mitral stenosis was defined by less than 1 cm² MVO by echocardiography. It has been sacredly followed in most countries where RHD is prevalent. But, as western data (often derived with eastern patients) redefined the cut off for severe MS to 1.5 cm² in recent years ,.Many of us are amused, rather confused.
Severe MS : Why it was made 1.5 cm² ?
I don’t know. Though, we in India, may not fully agree with this re-definition, there could be some good reason behind this. The bottom line is, we should not miss a functionally significant mitral stenosis, strictly adhering to the anatomical 1 cm² cut-off. After all, we all know, with years of experience in echocardiography ,in a funnel-shaped degenerated mitral valve, we can get whatever MVO we desire to report ! Same story for pressure half time, especially with tachycardia and little mitral regurgitation. We also realize the relationship between gradient and MVO is not at all linear.
So, what shall we do, when numbers play juggler game with us ? Let us go to the basics and learn to make a multi-parametric decision process.
Certain tips in assessing MS severity
1.When there is discrepancy in MVO always go with planimetry. If calcium is there MVO can be problematic; one may add a color flow in short axis to define exact flow borders in mid diastole.
2.If Doppler has multi phasic, humps we must take slopes that occur later in diastole for pressure half time. This is because, the initial rapid filling is influenced by early LV suction forces that may underestimate the MS severity.
3.In AF, always hesitate to diagnose moderate MS. Use a long cycle to measure pressure half time.
4.Finally, always have a look at the degree of pulmonary hypertension, LA enlargement, and sub-valvular disease before deciding if it is moderate or severe.
5.In pregnant women this one and a half MS is going to be really, really tricky to make a decision to Intervene. A fair rule of thumb is, If the mother crosses 20-24 weeks, whatever be the MVO , it is generally a good hemodynamic sign . (Except for the transient high risk period of the post natal uterine involution push and enhanced preload.) Having said that, we must realize , we are living in a near foolish and unrealistic era of demanding zero maternal complication even in high risk pregnancy. Many of us are compelled to do a seemingly unnecessary & risky PTMC during pregnancy due to the collective anxiety of cardio-obstetrics-patient team or a potential legal threat .
Other options
Dobutamine stress is an option , but many are hesitant to do.Stress testing that can be as simple as leg raising and bending 30 times while doing echo and check the gradient(?>20 mmHg)
What is new in hemodynamics of MS ?
There is something called low gradient severe MS (as in aortic stenosis). One must be aware of this. This often occurs in atrial fibrillation, where LA struggle to generate sufficient reservoir-stretch triggered flow gradient The other reason being presence of sub-clinical LV dysfunction hiking downstream pressure attenuating the gradient.(El Sabbagh A, Low-Gradient Severe Mitral Stenosis J Am Heart Assoc. 2019)
Final message
Though we are used to 1 cm² MVO cutoff , we can’t hang on to it strictly. Mind you, even a small gain in orifice can give a dramatic improvement in functional life. We have come across instances of splitting a mitral valve from a patient .8 to 1.5 cm² (technically they are still in severe MS), walking home briskly with a thankful smile. Same thing may happen for a patient with apparently moderate MS, right !
Posted in Uncategorized, tagged ase-posters, best-echocardiography-book, echo-manual, echocardiography, illustrative-echocardiography on December 15, 2023|
Learning resources in the web, has made the traditional methods of learning & teaching almost redundant.
American society of Echocardiography (ASE) has produced this 20 page PDF document, which covers the entire field of echocardiography , in an Illustrative format.

Take a print out, of this and stick in your lab (If you have space) for an Immersive experience. Hope, sharing this document here doesn’t violate any copyright issues.
Posted in Atrial fibrillation, tagged atrial strain in atrial fibrillation, diastolic dysfunction, dual doppler probe in atrial fibrillation assessment, e velocity variation in atrial fibrillation, echocardiography, HFpEF, how to assess diastolic dysfunction in atrial fibrillation?, single beat doppler echo on October 23, 2019|
Assessment of LV diastolic function primarily depends on the Doppler flow profile across the mitral valve and also to be noted are the 2D features of LA and LV for associated abnormality like LVH, LAE etc.
Why diastolic dysfunction assessment difficult in AF ?
Since most diastolic doppler mitral inflow parameters involve analysis of atrial contraction A wave, atrial fibrillation makes it difficult to assess diastolic dysfunction. Since we have only early diastolic velocity to assess, the changes confined to this E velocity is of paramount importance. This E velocity again is subjected to cycle length dependent alteration in both its acceleration and deceleration time , making things still more complex.
However, the following features help diagnose diastolic dysfunction in AF
*LA dimension is a very good sign of chronic elevation of LAP and diastolic dysfunction in the absence of mitral valve disease. However, AF can dilate the LA making it a less useful parameter. But, it should be noted in AF both RA and LA dilate together.So, a disproportionate LA>RA (or if RA is normal size ) could still be a marker of baseline LV diastolic dysfunction.
Reference
Posted in Cardiology-Arrhythmias, Cardiology-Echocardiography, Echo library and gallery, echocardiography, Interesting case study, tagged achalasia of cardia andleft atrial compression, cardiac mass, dysphagia and echocardiography, echocardiography, extra cardiac mass compressing left atrium, left atrial compression, reversible bradycardia, sinus bradycardia and achalasia cardia, sinus node dysfunction and achalasia cardia, tee, transthoracic esophago echocardiogram, transthoracic esophagoechogram on July 8, 2017| Leave a Comment »
A 50-year-old man was referred for dizziness, bradycardia and dysphagia .He was very clear in describing his symptoms and landed up in Gastro- enterology OPD , from there was referred to my clinic for cardiac work up . His ECG showed a sinus bradycardia HR of 48 /mt.

Echocardiogram revealed a structurally normal heart as we expected , but was surprised to spot suspicious shadow in para-sternal long axis view , beneath left atrium.
A well demarcated large mass compressing left atrium. Trans Thoracic Echocardiography may not be looking at the heart alone ,(Its technically Thoracic Ultrasound though we may refer it as Echocardiogram )
The Answer is none of the above
As I was wondering what it was, the staff nurse in charge threw a heavy folder with well worked up gastro Investigations.
That moment , diagnosis became obvious , without a need for further scrutiny to my medical acumen.

Note: The barium swallow of the Esophagus reveals the Intimate relationship between the food tube and the heart as it descends vertically downwards posteriorly . Realise , how the proximity of these two structures could confuse a physician when symptoms spill over on either way. (I would have expected a lateral view to show the compressive effect of Esophagus on the left atrium the radiologists felt its not important !)
Yes , it is Achalasia of the cardia , dilating the lower end of esophagus with fluid /mass effect , compressing the posterior surface of Left atrium.He underwent a myomectomy surgery.
Why bradycardia ?
There is well described esophago-vagal reflex reproducible by stressful swallow or balloon inflation in the lower end of esophagus at D7 level.(Ki Hoon Kang,Korean J Intern Med. 2005 Mar; 20(1): 68–71.)
Achalasia cardia is known to be associated with symptomatic bradycardia, dizziness, and rarely swallow syncope,though this patient didn’t have a classical syncope.The bradycardia is probably due to high vagotonia, (Hugging effect on posterior surface of heart known for rich innervation of vagus.) . Complete reversal of bradycardia after esophago -gastric surgery is expected.
Implication for cardiologists
There has been instances of patients with esophageal syncope and reflex bradycardia getting permanent pacemaker therapy. I think , clinical or sub clinical esophageal disorders should be included in the work bradycardia before labelling them as intrinsic sinus node dysfunction .(Ref 1,4)
Final message
The field of Cardiology is often referred to as a super specialty atleast in India . I disagree with it strongly. Cardiologists are neither super(eme) nor special .We need to be reminded its afterall a sub-specialty of Internal medicine and each specialist should undergo retro-training in medicine periodically .This patient is a typical example of a gastric problem entering the domain of cardiac Imaging.Strong foundations in symptom analysis and some degree of medical curiosity will enable an occasional cardiologist to make a correct diagnosis belonging to a remote foreign specialty.
Reference
1. Palmer ED. The abnormal upper gastrointestinal vagovagal reflexes that affect the heart. Am J Gastroenterol. 1976;66:513–522. [PubMed]
2.Armstrong PW, McMillan DG, Simon JB. Swallow syncope. Can Med Assoc J. 1985;132:1281–1284. [PMC free article] [PubMed]
Posted in Uncategorized, tagged can technician interpret ecg, ECG, echocardiography, who should do echocardiography ? on July 20, 2013| 1 Comment »
A Cardiologist will never accept the diagnosis , if a technician reports a ECG as normal in a patient with chest pain . . .
While , the same cardiologist gleefully accepts an echocardiogram done by a technician and treats the patient without verifying the veracity of the finding !
Why ?
Some where along the cardiology training , we have been made to believe Interpreting Echo Images does not require serious medical knowledge . . . but we strongly believe ECG cannot be read by technicians however well they are trained .(In-spite of the fact , Echo images are highly dependent on the person who does it , while ECG wave forms are totally independent of the person who record it ! )
ECG, still has a prestigious place in cardiologist’s mind , while Echo is often considered an inferior Investigation. Many of us consider ECG interpretation as a brainy work while Echo image acquisition and interpretation is perceived a dumb job* !
Lastly , probably most importantly , performing Echo is a time intensive process for the present day cardiologist who’s hands are tied with catheters and guide-wires .He has little time for the meanly echo . . . hence ready to compromise on the quality .
* With due respects to all non invasive cardiologists (That includes the author !)
Final message
I would think it is fundamentally inappropriate for technician to report Echocardiogram (Of-course they may record it ) . Unfortunately , for some reason this practice is continued in many parts of world .
Posted in cardaic physiology, Cardiology -unresolved questions, Echo library and gallery, echocardiography, tagged AML movement M shaped, echocardiography, M MODE CHO AML, rare mode echo, trifid m mode echo of aml, trifid mitral inflow doppler on January 31, 2013| Leave a Comment »
Anterior mitral leaflet (AML) is an unique structure in the heart .It is the fastest moving structure inside the heart . It is the first structure visualised by echocardiogram by Elder and Hertz in early 1950s .
While AML is known for vigorous motion , the PML motion is subdued . By tradition AML shows a motion which resembles alphabet M .
But AML is not be taken lightly . It can change it’s motion not only in pathological states but also in health . One such pattern is trifid motion of AML . Following is a Echo Image in a perfectly normal Individual .
Possible mechanisms underlying Trifid motion of AML
Does trifid AML motion result in Tri-phasic doppler flow as well ?
Mitral valve filling is classical E and A .
This usually correspond to M pattern of anatomical AML motion .
Do the anatomy goes hand in hand with physiology ? Will the mid diastolic AML drag result in augmented flow ?
We are looking at this phenomenon .
Posted in echocardiography, Top ten in cardiology, tagged best web site for echocadiography, echocardiography on September 30, 2012| Leave a Comment »
Learning and sharing of knowledge is one of essential qualities of that make the man kind unique.
But not everyone is ready to do that . A cardiologist from Paraguay shows the way . . .
Probably a model web site for all academicians .It exemplifies , how a medical web site is to be created and presented .This one is for learning echocardiography .
Though the author calls , it as basics it has fairly advanced contents , so it should be useful at levels .
With due courtesy to Dr Derliz Mereles I am linking his web site in my blog .
Posted in Cardiology teaching websites, Cardiology-Land mark studies, valvular heart disease, tagged 3d echo real time, 4d echocardiography, echocardiography, mitral valve echo rt3de, mitral valve scallop, mvps, p2 prolapse, three dimensional echo of mitral valve anatomy on June 3, 2012| Leave a Comment »
Who said knowledge comes at a cost . Here is a great resource . Everything about 3D echo
A sample of 3D echo evaluation of mitral valve anatomy
Posted in Uncategorized, tagged cardiac risk assement before surgery, echocardiography on February 29, 2012| 3 Comments »
Can you safely rule out heart disease before non cardiac surgery without echocardiography ?
Yes , in most situations . Experience suggest If the clinical examination is normal , ECG and X ray do not show any abnormality , significant heart disease is ruled out 95/ 100 times.
Please note : ECG and X-ray can not R/O Coronary artery disease by any degree of specificity .Echo cardiogram also miserably fails to predict future CAD. But EST / TMT does this very efficiently!
So where does the echo comes in the routine protocol in the screening of heart disease* ?
“No where” to be precise. It is only a gimmick . But many physicians and anesthetists are obsessed with echo estimated LV EF % They invariably ask for pre operative echo for cardiac risk stratification.
* On the other hand EST has a strong case for inclusion as a routine screening test before surgery.
What about diastolic dysfunction ?
ECG and X ray will not miss a manifest myocardial disease . However concealed diastolic dysfunction can not be detected without echo. It is very common to detect early forms of diastolic relaxation abnormalities in echo . Significance of this is not clear especially if it is grade 1 . In this situation patient’s functional capacity comes to our rescue. In a non functional patient any degree of diastolic dysfunction may increase the pulmonary capillary wedge pressure. These patients must be monitored and fluid administration should be be judiciously used.
Final message
Echocardiography rarely comes* in the routine scheme of things in the pre -operative cardiac risk assessment.
Summary
First question to ask before non cardiac surgery is about the symptoms and functional capacity . ( Do you climb 3 floors ? Walk 6 km /hr . lift 20kg over a flight of stairs , objectively walk 9 mts on treadmill with std Bruce) If he is asymptomatic and his functional capacity is good , for all practical purposes he will be fit for surgery in cardiac point of view .
Next , we need to look the ECG and X ray chest . If one of them shows some evidence for chamber enlargement / q waves etc ,an echocardiography is ordered .
If you really suspect CAD one should go for EST or doubtamine stress ECHO.
* Cardiologist lack professional freedom in new age medicine :
In this funny medical world , a cardiologist can not do what he wants to do . I have encountered surgeons and anesthetics refusing to take a patient for surgery without knowing the ejection fraction ! Once when I gave a surgical fitness without taking an echo there was a furore from the corporate desk of a big hospital . How can you make decision without these modern gadgets they seemed to ask ! Future looks lovely for cardiology !