We wish, our understanding about cardiac contractile physiology is deep and nearly complete. Heart is an irreversibly coupled electro-mechanical organ , right from the fetal days until the final heart beat. In myocardial pathology, the genesis and sustainability of ventricular arrhythmia are intricately related to the degree of LV dysfunction of any cause.
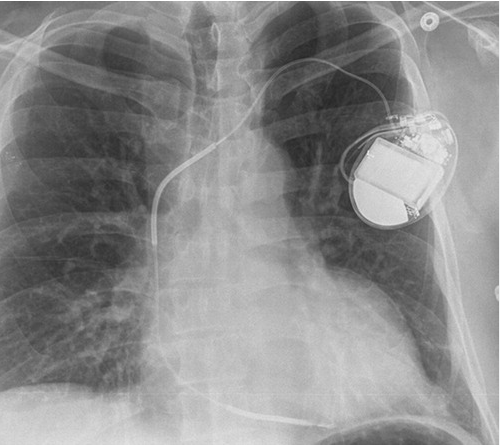
SCD is the leading cause of mortality in heart failure. Tackling SCD was in God’s domain, until the brilliance of Dr. Michel Mirowski shrunk the defibrillator and implanted it under the chest in 1980. (Dr. MM’s s a unique and inspiring story, from Poland amidst the holocaust times, right up to his invention at Johns Hopkins)
Why ICD for SCD ?
Beta blockers and Amiodarone remain good options for mitigating SCD. (Of course, Amiodarone has a huge baggage of side effects.) But, as you know machines always beat drugs. After multiple RCTs, we found any severe LV dysfunction (EF <30%) requires an ICD to reduce SCD. Though MADIT trial required an inducibility of VT, MADIT-2 told us that just the presence of LV dysfunction is sufficient.
Since then, ICDs have proliferated globally, of course with multiple collateral issues. As we navigated the cardiac EP terrain further, we found that all is not well. ICDs faced some foundational questions regarding its utility value vs. risk . ICD explanation epidemic in the past was a true story. Still, Mirowski”s electrical kid survived the test of time and evolved with great technological innovations from companies like Medtronic, Guidant, Abbot etc. It has, now grown into 45 year old wonder device, that can wake up the heart from death . (Wish ,the Nobel committee has Dr Mirowski’s name in their podetial posthumous prize list)
ICD usage with reference to DCM sub types
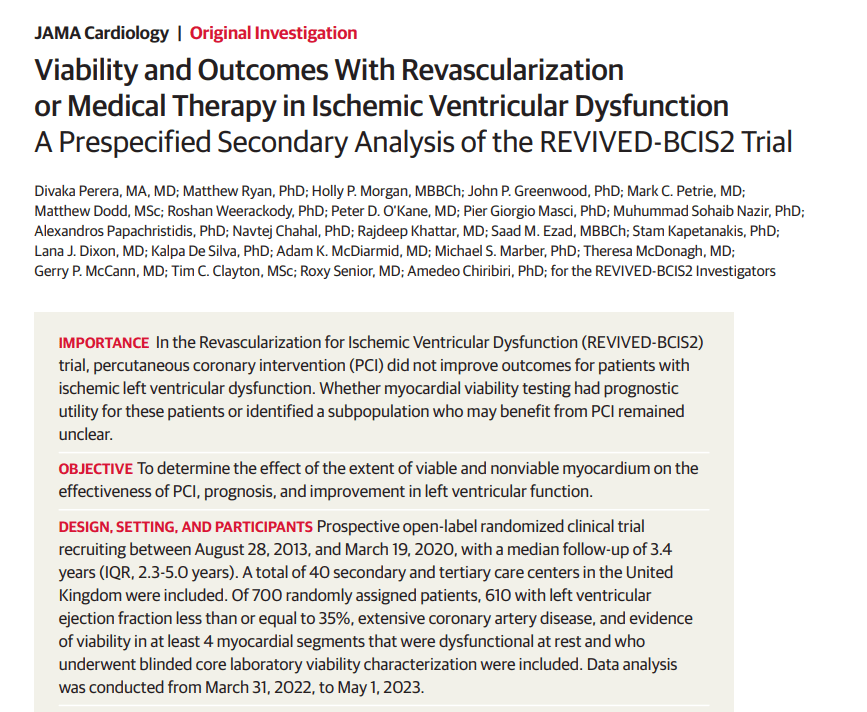
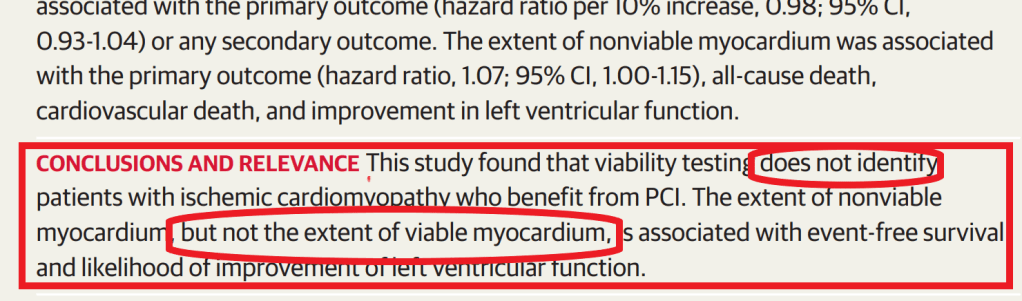
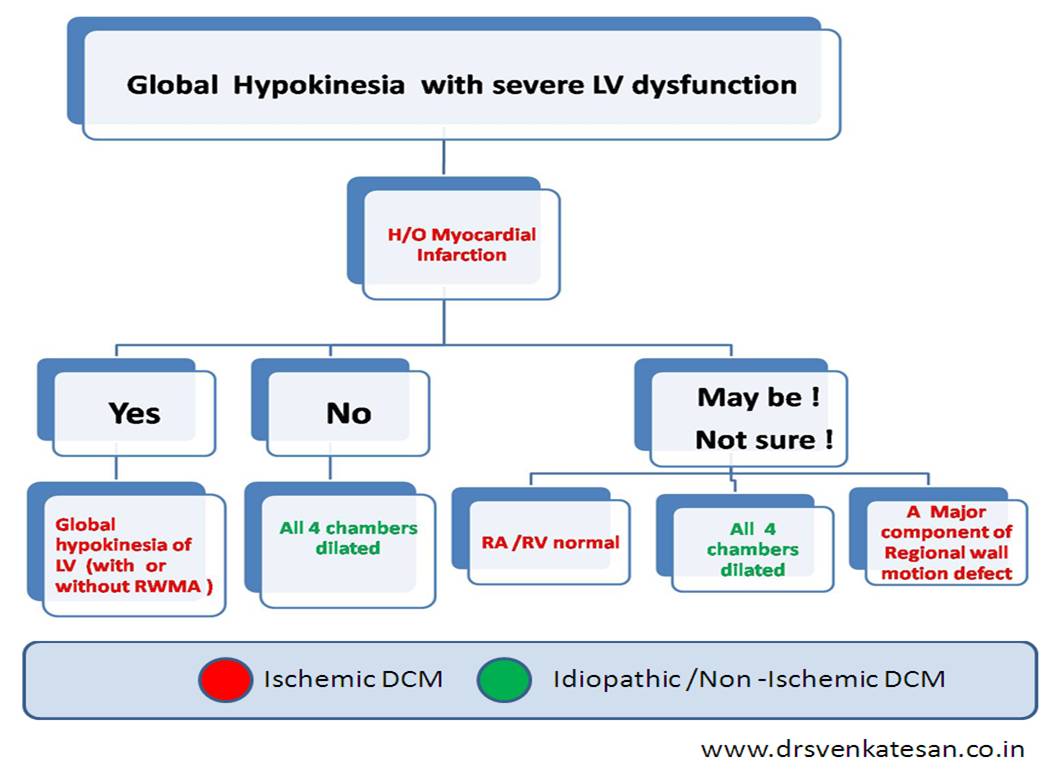
One factor frequently debated about ICD is its efficacy with reference to the etiology of LV dysfunction. Many studies indicated this factor could tilt the balance of risk to benefit of ICD in a critical way. ICDs are more useful in Ischemic DCM than non ischemic DCM is a recently observed penomenon ,though we are not sure yet . SCD-HeFT trial (NEJM 2005) did show some benefits in N-DCM, but it was only in class 2 stage. Then came the DANISH study, which made us strongly believe ICDs in Non-Ischemic DCM are not a really useful intervention. (N Engl J Med 2016; 375:1221-1230)
Why ICD doesn’t work well in NDCM ?
Since IDCM patient had more SCD events , ICD is more likely to be useful in ischemic DCM than non ischemic is a distinct possibility (Higgins AY, . Am J Cardiol. 2020)
The un-disputable fact is ischemic DCM has a target to treat, though it is termed as cardiomyopathy. While most of non-ischemic DCM are truly global muscle disease with primary or secondary with known or unknown disease process, unless we are able to correct the etiological factor, these patients are not going to do well in spite of ICD.
The differentiation between DCM and NDCM itself is not a simple task. Overlaps do occur. (An important clue is NDCM involves both ventricles equally and subendocardial sparing almost always suggests NDCM)
Final message
It seems to be a fact, ICD are less useful in NDCM. The simple reason could be we can address the ischemia a potential arrhythmic target by some form of revascularization in IDCM. The second reason is, NDCM is a progressive primary muscle disease.
Still, our understanding is largely incomplete. ICDs don’t exhibit partiality. By default, they try to give a new lease of life to any episode of pulseless VT/VF whether it is from IDCM or NDCM. (Please remember we don’t deny an ICD for a sarcoid cardiomyopathy or end-stage HCM just because they are non-ischemic. in origin )
Post-amble
An unfriendly fight between CRT & ICD
The science of LV dysfunction and the need for ICD got complicated when CRT entered the scene a decade ago. CRT is indicated when a LV is dilated with poorly coordinating contractions due to conduction system malfunction, that stretch the QRS complex either LBBB or monophasic RBBB or combination both BBBs(Masquerading)
Since, the indication between ICD and CRT overlapped, industry guys taught us some cardiology lessons, They offered the option of fusing the two together and called it CRT-D & CRT- P. Please note CRT-P is nothing but the glorified version of plain old CRT (The P could mean either the dual /BV or the mono ventricular (RV) default back up pacing.)
The choice between CRT -P and D has taken more curious turns. Since we are not clear whether the incidence of SCD is reduced by CRT or ICD. This paper from Egypt address this issue in an exemplary manner. (Ref 4).
Now, there are more than handful of papers that show CRT-P per se can reduce the SCD events significantly by reverse re modeling of LV and improvement of LV function. Currently, we have started to believe CRT-D may not be indicated in many and could in fact add more electrical side effects.
It is ironical, currently the issue of in-appropriate ICD/CRT-D implantation appears more important than the well known adversary of inappropriate shocks. Both of them needs some meaningful attention. It is worthwhile to to note ,If we address the former the later issue cease to exist. Let the global EP think tank introspect and to refine and redefine the Indications of CRT-D.
Reference
DANISH 10 year follow up re-confirms it
4. CRT -P vs CRT-D