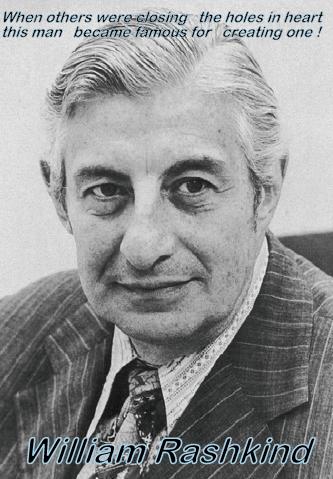
Who is the father of interventional cardiology ?
William Rashkind a cardiologist from Children’s hospital, Philadelphia in 1966 probably is the first person who thought it was indeed possible to use a wire and balloon as cardiac therapeutic intervention .When surgeons were groping in dark with sick cyanotic new borns with dTGV , He along with Miller executed their idea.
It was published in JAMA
How the Rashkind has revolutionized our approach to congenital heart disease is evident from the current guidelines in 2011.
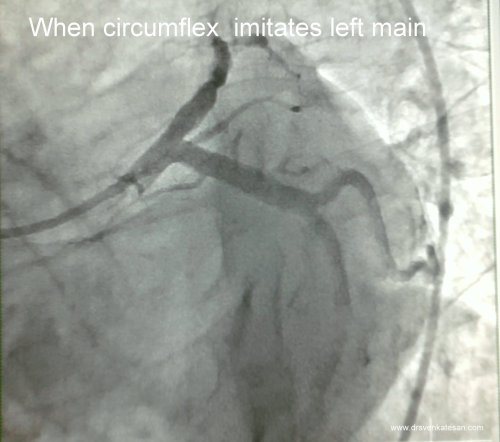
The procedure has since evolved with improving hardware and we are able to ferry a blade into the IAS for cutting .
Current recommendations for Atrial septostomy
It is primarily useful
1. Atrial septostomy to enhance atrial mixing (eg, transposition of the great vessels with restrictive/intact atrial communication) or to decompress the left atrium
2.During Extra corporeal membrane oxygenation (ECMO) to decompression of left atrial hypertension
3.If there is poor cardiac return from ECMO circuit low venous saturations (Class 1 Evidence C)
It may also be tried in (Class 2 )
1. Hypoplastic left heart syndrome with restrictive atrial communication.
2. Static balloon dilation of l synthetic / bioprosthetic IAS (eg, Gore-Tex)
3. Tricuspid atresia with restrictive atrial communication
4 .Pulmonary atresia with intact IVS
5. TAPVC with restrictive atrial communication.
6. Primary pulmonary hypertension / Eisenmneger VSD/PDA .(Occasionally useful )
Reference
http://circ.ahajournals.org/content/123/22/2607.full.pdf+html