Atherosclerosis probably ranks first among all human diseases that cause maximum suffering to mankind.Since it is a disorder of blood vessel it has an easy access to every vital organ in our body to inflict the damages . Histo pathologically , atherosclerosis is an all in one disorder where inflammatory , degenerative and lipid injury collectively contribute to the disease progression. Diabetes and hypertension play a vital amplification role.
Atherosclerosis begins very early in life as fatty streaks in every individual and takes different avatars ( or remain indolent) depending upon the risk factors and life style.
How to estimate plaque burden ?
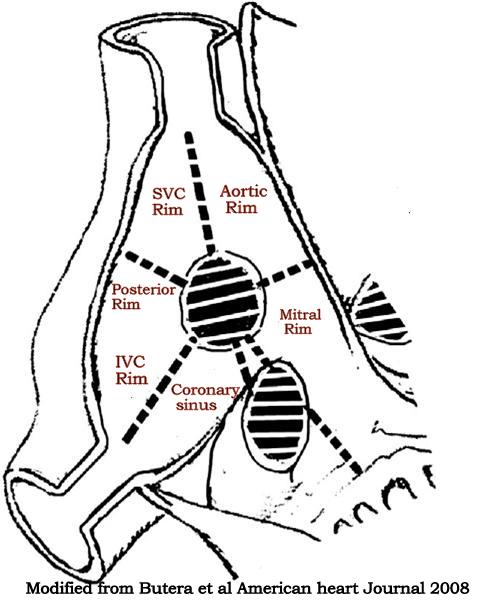
It has always been a difficult task to estimate the atherosclerotic plaque burden inside the coronary arteries.The fundamental flaw for many years is , we always thought if there is a plaque it must encroach into the lumen.
Coronary angiogram , has become the default investigation in clinical cardiology . Since it can visualize only the coronary lumen , this flaw got further curious with skewed interpretation as well.
When things were as it is . . . Glagov suggested , what could possibly be the most important concept in the interpretation of coronary angiogram .
The concept suggested the atherosclerotic process could actually spread within the vessel wall in a predictable manner .

What determines a plaque to either grow into the lumen or grow away from the lumen?
If we could decode the mechanism of direction of plaque growth we will probably conquer the atherosclerosis at least by mechanical means . The implications are too many.
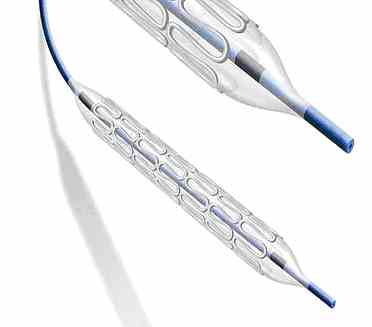
A stented coronary artery may be re-engineered to grow the atherosclerosis towards the adventia .This could grossly reduce the incidence of restenosis.
Further , in post Glagov days we realised mechanical factors like plaque stiffness, eccentricity , plaque mass effect, drifting , lipid core density, medial lysis , elasticity of elastic lamina all could determine the plaque movement.
Why compensatory lumen enlargement does not occur in some lesions ?
We do not know the exact reasons . We may call it a fate . . . shall we ?
Curious blessing : Atherosclerosis for some unknown reason blesses a few with coronary artery dilatation rather than narrowing .
This is called coronary ectasia . Medial necrosis , weakness of internal elastic lamina or destruction paves way for plaque shift towards the adventia . It is estimated , if the medial necrosis occurs in at least 50 % of circumference of vessel wall it will result in ectasia .And paradoxically if the media shows resistance the plaque grows into the vessel wall.
Endoleak and Glagovian phenomenon.
Endo leak is the Achilles heel of endovascular intervention . In fact , many would consider it as a dignified terminology for graft failure . Endo Leak occurs when the artery outgrows the stent graft and bllood starts collecting in the graft vessel -wall interface . When the scaffold is placed within the lumen , one may wonder how it is going to prevent the artery dilatation . (Which is basic defect in any aneurysm}In fact , the aneurysm does continue to grow along with centrifugal atherosclerotic forces , possibly by Glagovian phenomenon .
This makes it obvious endo- leak is a distinct threat in every vascular intervention.
Final message
Most cardiologists think their ultimate job in this world is to deploy a stent deep inside a LAD or RCA. While a few others indulge in more exotic adventure of crushing a plaque , trap the debris and catch it with a with a basket .
There are bigger and bigger blind areas in the vessel wall , infiltrated with deadly atherosclerosis which is conveniently ignored .If only we realize this fact , we can move forward in our war against coronary atherosclerosis.
Of course the good old medical interventions . . . exactly try to address these issues . Let us think straight , and not succumb to glamor in cardiology !
http://heart.bmj.com/content/84/5/461.extract
Read Full Post »