Any structure which has a foundation on which it stands is generally called base or basement. By tradition base is synonymous with bottom .Ironically , for heart this rule does not apply. This is the core area of confusion. The heart is a complex shaped 3D organ with multiple surfaces with 4 chambers connected each connected to its own great vessel .
We know heart is simply suspended by these vessels inside the middle mediastinum and anchored with ligamentous attachment to chest wall, diaphragm through pericardium .
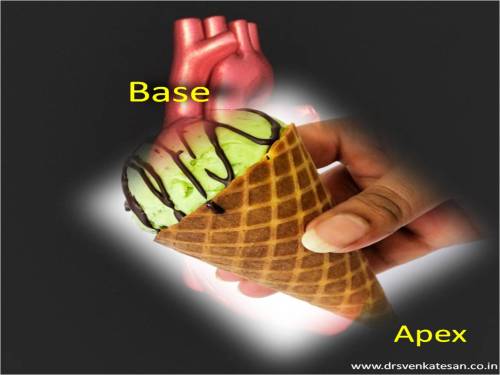
Now, traditionally the heart was thought to be cone like stricture with apex located near the left mid clavicular line .
If there is an apex there must be a base .So , we reasoned the highest and farthest part of the heart must be the base . Paradoxically , this base is at the top , and not in the traditional sense of bottom .
Like wise , during auscultation the events in the base represent the great vessel and semilunar activity (Anteriorly )
Baseless base
Clinical base is not the anatomical base . When a patient lies on his back essentially the atria and posterior aspect of ventricles form the base . In erect posture the diaphragmatic surface becomes the true anatomical base of the heart .
Further confusion during Echocardiography
It is well known , basal LV function is a critical determinant of LV function .But we should be very clear what area we are talking about ! Basal aspect can lie either superior , inferior , anterior even posterior surface of left ventricle .(It took me years to realise this simple fact !)
Similarly basal septum can mean either a LAD zone or even RCA zone one has to specify basal anterior septum to define LAD zone ischemia .
(Please note , this is contrast to clinical cardiology where the base of the heart refers only to anterior aspect of heart ! )
FInal message
Calling a particular portion of the heart as base would be an anatomical misnomer . This nomenclature is based , more by tradition and our faulty perception .(As visualized by anatomists and pathologists )
We have come a long way from the Da Vinci days. Modern cardiologists with sophisticated imaging techniques would like to call the basement of heart differently in the future and correct the nomenclature issues.